Arthritis affects millions worldwide, transforming simple daily activities into challenging tasks. At PrimeCare Orthotics & Prosthetics, we understand the profound impact joint inflammation has on your quality of life, and we’re here to help.
Our comprehensive approach combines cutting-edge orthotic solutions with personalized care plans to address arthritis symptoms from multiple angles to restore mobility and reduce pain effectively.
What Is Arthritis?
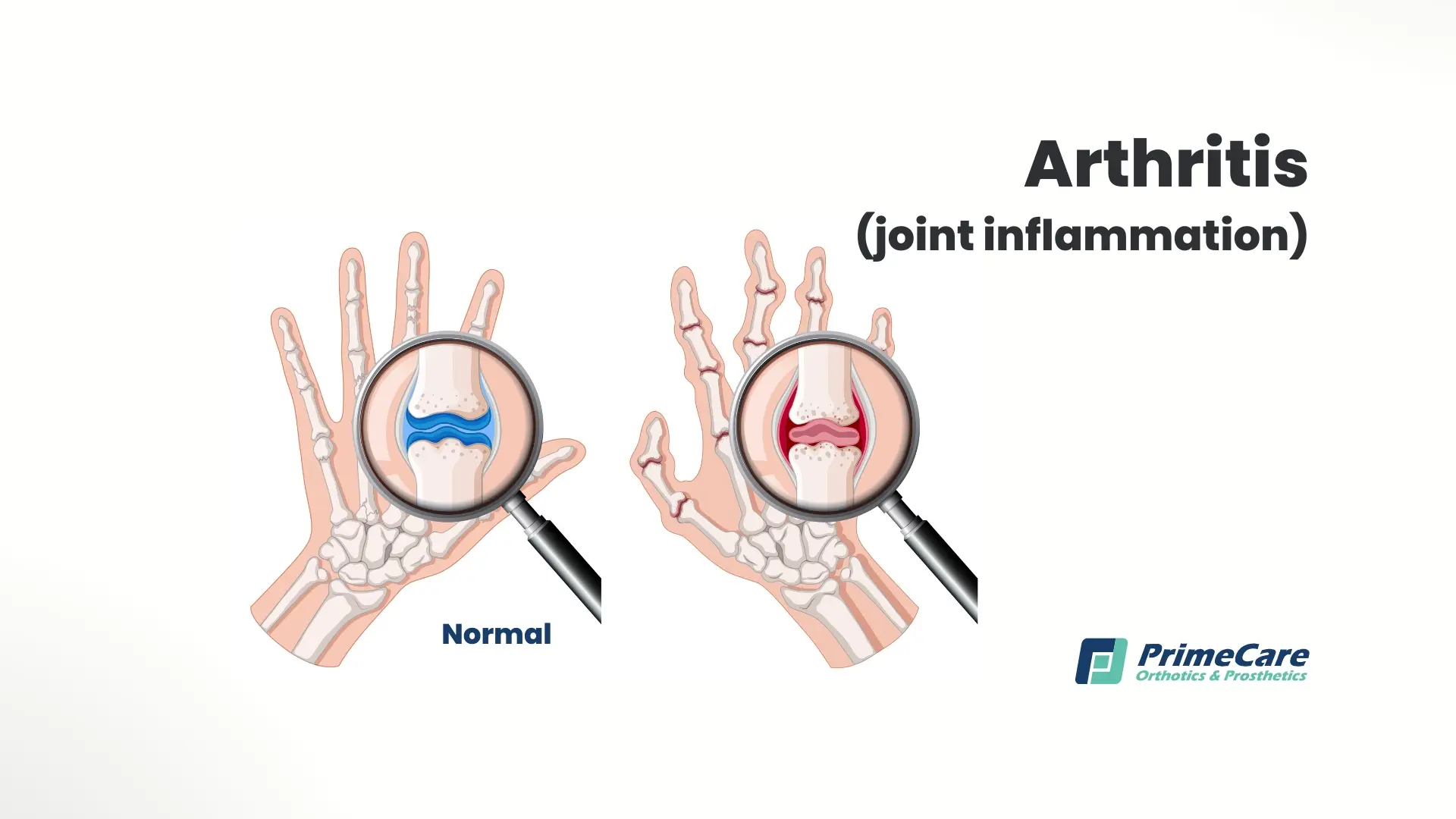
When most people think of arthritis, they envision stiff, painful joints that worsen with age. However, this complex condition encompasses far more than simple wear and tear. Understanding the true nature of arthritis is the first step toward effective management and treatment.
Arthritis consists of over 100 conditions causing joint inflammation, pain, and stiffness. This degenerative condition affects the cartilage cushioning your joints, leading to bone-on-bone contact that triggers inflammation and discomfort.
The disease progressively damages joint structures, including surrounding ligaments and muscles, resulting in reduced range of motion and functional limitations. While commonly associated with aging, arthritis can affect people of all ages. It manifests as either inflammatory conditions like rheumatoid arthritis or mechanical wear-and-tear disorders like osteoarthritis.
Arthritis Prevalence: A Growing Health Concern
The widespread impact of arthritis on global health cannot be overstated. As our population ages and lifestyle factors evolve, understanding the scope of this condition becomes increasingly crucial for public health planning and individual awareness.
Arthritis ranks as the leading cause of disability globally, affecting:
- Over 54 million adults in the United States
- 1 in 4 adults experience activity limitations due to arthritis
- Women are disproportionately affected (26%) compared to men (19%)
- Prevalence increases significantly with age, affecting 50% of adults over 65
Different Forms of Arthritis: How to Identify Your Type

Not all arthritis is created equal. Each type has unique challenges, progression patterns, and treatment requirements. Identifying your specific arthritis type properly can help you develop an effective management strategy.
Osteoarthritis (OA): The Wear-and-Tear Arthritis
Osteoarthritis is the most prevalent form, affecting over 32.5 million US adults. This mechanical condition develops when protective cartilage gradually wears down, typically affecting:
- Knees: Supporting body weight leads to progressive cartilage loss.
- Hips: Ball-and-socket joint deterioration causes groin and thigh pain.
- Hands: Finger joints develop characteristic bone spurs (Heberden's nodes).
- Spine: Vertebral disc degeneration triggers back pain and stiffness.
OA typically develops asymmetrically, affecting one side more severely than the other. Morning stiffness usually resolves within 30 minutes, which distinguishes it from inflammatory types.
Rheumatoid Arthritis (RA): When Your Immune System Attacks
Unlike osteoarthritis, rheumatoid arthritis is an autoimmune condition affecting 1.5 million Americans. The immune system mistakenly attacks the synovium (joint lining), causing:
- Symmetrical joint involvement: Both hands, knees, or feet affected equally.
- Systemic inflammation: Fatigue, fever, and organ involvement are possible.
- Progressive deformity: Untreated RA leads to joint destruction.
- Extra-articular manifestations: Eye inflammation, lung scarring, heart problems.
RA typically strikes between the ages of 30-60, with women three times more likely to develop the condition. Early aggressive treatment prevents irreversible joint damage.
Psoriatic Arthritis: Skin and Joint Connection
Affecting 30% of psoriasis patients, psoriatic arthritis combines skin symptoms with joint inflammation. Characteristics include:
- Sausage digits: Entire fingers or toes swell dramatically.
- Nail changes: Pitting, separation from the nail bed.
- Enthesitis: Inflammation where tendons attach to bone.
- Varied patterns: Can mimic RA or affect the spine like ankylosing spondylitis.
Gout: The Crystal-Induced Arthritis
Gout results from uric acid crystal deposits in joints, causing:
- Sudden, severe attacks: Often starting at night.
- Big toe predilection: The First metatarsophalangeal joint is commonly affected.
- Dietary triggers: Alcohol, red meat, seafood.
- Male predominance: Until menopause provides female protection.
Additional Types of Arthritis

Juvenile Idiopathic Arthritis (JIA)
- Affects children under 16
- Multiple subtypes with varying prognoses
- Can impact growth and development
Lupus Arthritis
- Part of systemic lupus erythematosus
- Non-erosive but extremely painful
- Accompanies other organ involvement
Septic Arthritis
- Medical emergency requiring immediate treatment
- Bacterial infection within the joint space
- Rapid joint destruction without antibiotics
Ankylosing Spondylitis
- Primarily affects the spine and sacroiliac joints
- Leads to spinal fusion if untreated
- Strong genetic component (HLA-B27)
Recognizing Arthritis Symptoms Early

The earlier you recognize symptoms, the easier it is to improve treatment outcomes. While each arthritis type has unique features, certain warning signs warrant immediate medical attention to prevent permanent joint damage.
Primary indicators include persistent joint pain, particularly after activity or prolonged rest periods. Morning stiffness lasting over 30 minutes often signals inflammatory arthritis. Affected joints may exhibit visible swelling, warmth, and redness. Patients often report grinding sensations (crepitus) during movement, decreased flexibility, and joint instability. Advanced cases may present with joint deformities, bone spurs, and significant functional limitations that impact daily activities.
Here are some red flag symptoms requiring urgent evaluation:
- Sudden and severe joint pain with fever
- Rapid joint swelling with skin color changes
- Complete inability to move the affected joint
- Multiple joints that become painful simultaneously
What Causes Arthritis to Develop?
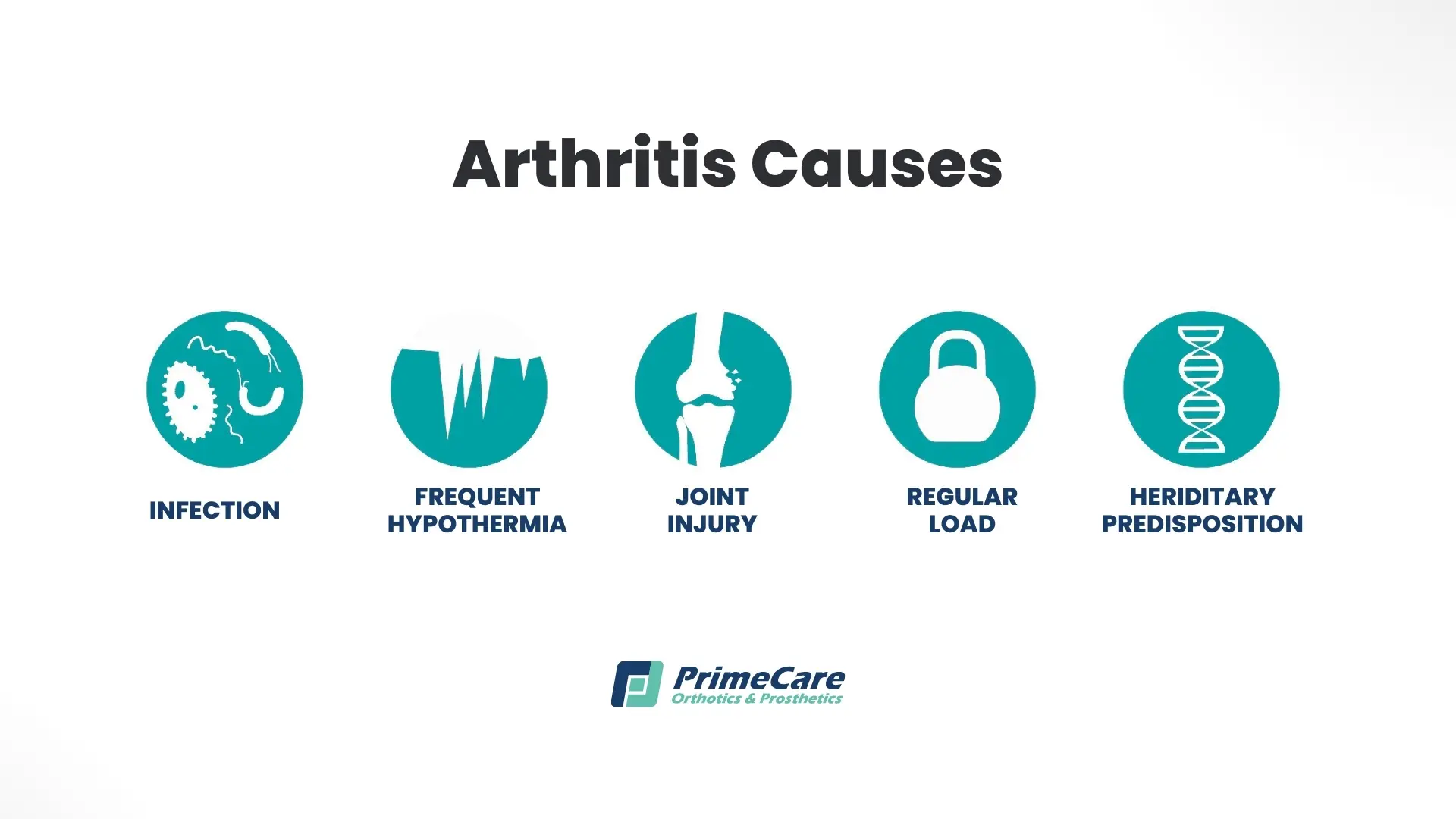
Arthritis develops through various mechanisms depending on the type. For example, osteoarthritis results from cumulative joint stress, previous injuries, and natural aging processes breaking down protective cartilage. Rheumatoid arthritis stems from autoimmune dysfunction, where the body attacks healthy joint tissue. Contributing factors include genetic predisposition, obesity that places excess stress on joints, repetitive occupational movements, and certain infections triggering reactive arthritis.
Environmental triggers include:
- Workplace exposures to silica or asbestos
- Smoking triggers RA in genetically susceptible individuals
- Viral infections like Epstein-Barr virus
- Gut microbiome imbalances affecting immune function
Who's at Risk for Developing Arthritis?
Arthritis doesn't discriminate, but certain factors significantly increase your likelihood of developing joint disease. Understanding your personal risk profile enables targeted prevention strategies and early intervention when symptoms first appear.
Non-modifiable risk factors:
- Age: Cartilage naturally thins and weakens over time.
- Gender: Women face 2-3 times higher RA risk due to hormonal influences.
- Genetics: HLA genes strongly predict inflammatory arthritis development.
- Previous injuries: Post-traumatic arthritis develops in 12% of osteoarthritis cases.
Modifiable risk factors:
- Weight: Each pound of excess weight adds four pounds of knee joint stress.
- Occupation: Jobs requiring repetitive kneeling, squatting, or heavy lifting.
- Sports participation: High-impact activities without proper conditioning.
- Muscle weakness: Inadequate joint support accelerates cartilage breakdown.
- Dietary factors: High purine foods that trigger gout attacks.
Potential Complications of Untreated Arthritis

Untreated arthritis progressively damages joint structures, leading to permanent deformities and disability. Chronic inflammation increases cardiovascular disease risk, particularly in rheumatoid arthritis patients. Severe joint damage may necessitate replacement surgery. Additionally, arthritis-related mobility limitations contribute to muscle atrophy, osteoporosis, and increased fall risk.
Psychological impacts include:
- Depression affects 20% of arthritis patients
- Anxiety from unpredictable pain patterns
- Social isolation due to activity limitations
- Sleep disturbances from nighttime discomfort
How Is Arthritis Diagnosed?
A comprehensive arthritis diagnosis starts with a detailed medical history documenting symptom onset, patterns, and aggravating factors. Physical examination assesses joint tenderness, swelling, range of motion, and deformities.
Laboratory investigations include:
- Inflammatory markers (ESR, CRP) indicating disease activity
- Rheumatoid factor and anti-CCP antibodies for RA diagnosis
- HLA-B27 testing for ankylosing spondylitis
- Uric acid levels that evaluate gout
Imaging studies reveal:
- X-rays showing joint space narrowing and bone changes
- MRIs detecting early cartilage damage and inflammation
- Ultrasounds identifying synovitis and erosions
- DEXA scans assessing associated osteoporosis
Joint fluid analysis differentiates inflammatory from non-inflammatory arthritis while ruling out infection.
Comprehensive Treatment Approaches for Arthritis
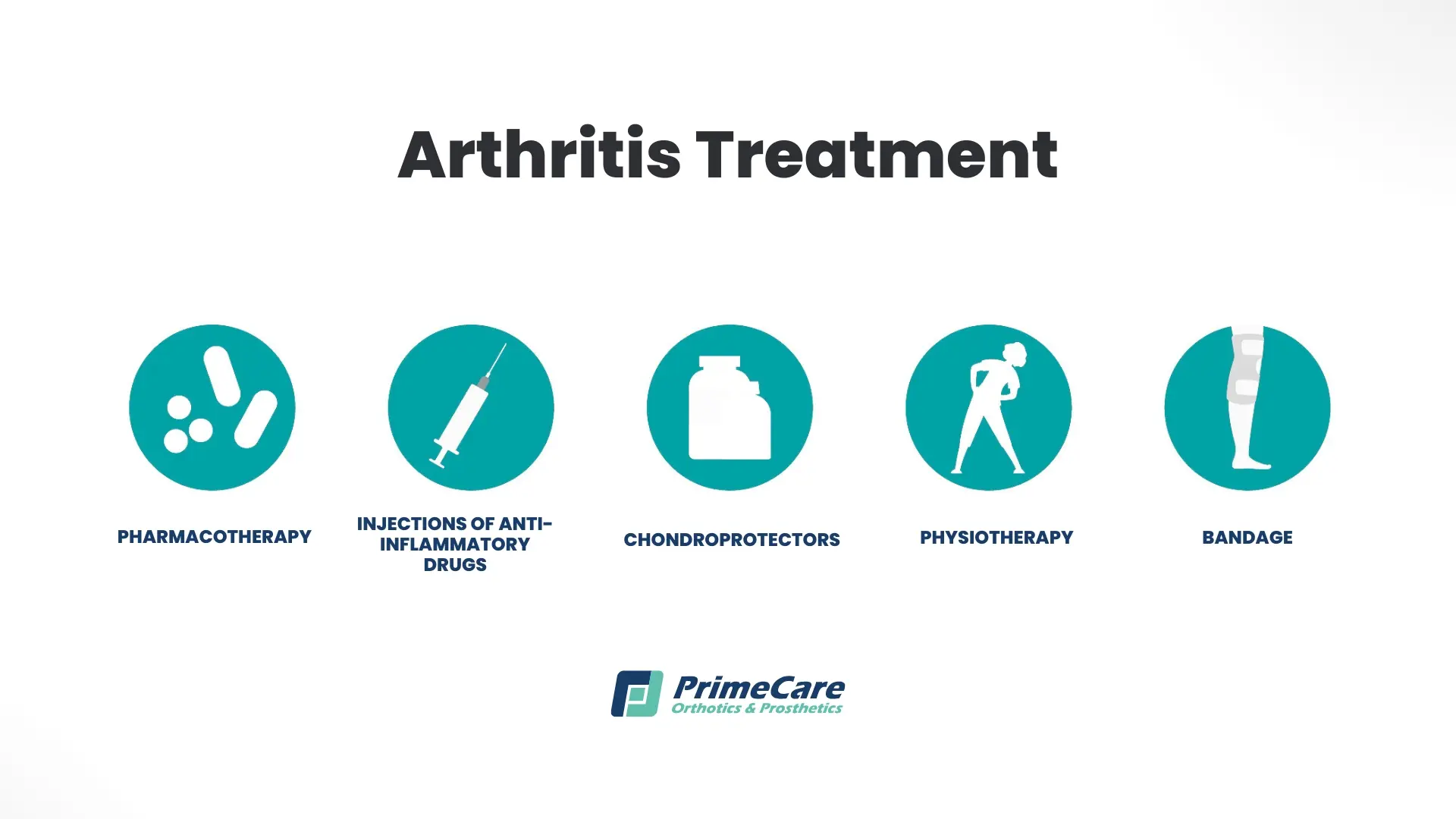
Modern arthritis management combines multiple therapeutic modalities tailored to individual needs. For treatment to be successful, it needs to address both symptoms and underlying disease processes while maintaining optimal function.
Medication Management
Anti-inflammatory medications provide symptom relief through oral NSAIDs or topical preparations for localized pain. Disease-modifying antirheumatic drugs (DMARDs) slow RA progression, while biologic agents target specific inflammatory pathways. Corticosteroid injections offer temporary relief for severe flare-ups.
Physical and Occupational Therapy
Specialized exercise programs strengthen supporting muscles while maintaining joint flexibility. Therapists teach joint protection techniques and recommend assistive devices for daily activities. Aquatic therapy is another way to reduce joint stress while building strength.
Orthotic Interventions
Custom orthotics and braces provide crucial support and redistribute pressure away from affected joints. These devices stabilize joints, reduce pain, and improve function during daily activities. Properly fitted orthotics can slow disease progression by correcting biomechanical abnormalities.
Surgical Options
In advanced cases, arthroscopic procedures can remove damaged tissue. Joint replacement surgery is for severely deteriorated joints. When replacement isn’t suitable, fusion surgery stabilizes painful joints.
Complementary Approaches
Weight management is a simple way to reduce joint stress, while dietary modifications incorporating anti-inflammatory foods support overall joint health. Acupuncture, massage therapy, and heat/cold applications provide additional symptom relief for many patients.
Specialized Orthotic Solutions for Arthritis

Orthotic interventions offer non-invasive, effective management for arthritis across all affected joints. At PrimeCare, our comprehensive approach addresses specific biomechanical needs while accommodating individual limitations. Here’s how we can help.
Knee Orthotics
An arthritis knee brace provides essential stability for affected knees, reducing pain during weight-bearing activities. Our custom knee brace for arthritis options include:
- Unloader braces that shift pressure from damaged compartments
- Hinged supports that prevent hyperextension
- Compression sleeves that reduce swelling and improve proprioception
Foot and Ankle Support
Insoles for arthritis address biomechanical imbalances contributing to joint stress. Our arthritis foot insoles feature:
- Customized arch support to redistribute pressure
- Metatarsal pads help relieve forefoot arthritis
- Heel cushioning protects posterior joints
Foot orthotics for arthritis provide comprehensive support through:
- Custom-molded designs matching individual foot contours
- Shock-absorbing materials reducing impact forces
- Accommodations for existing deformities
An arthritis ankle brace stabilizes affected joints while permitting controlled motion. Orthotics for ankle arthritis incorporate rigid or semi-rigid shells, limiting painful movements.
Hand and Wrist Solutions
A hand brace for arthritis maintains proper joint alignment during activities. Options include:
- Resting splints for nighttime use
- Functional braces that permit controlled movement
- Thumb spica supports for basal joint arthritis
An arthritis wrist brace reduces strain on inflamed joints through:
- Adjustable compression levels
- Removable stays for customized support
- Breathable materials for extended wear
Specialized Orthotic Features
Orthotics for arthritis in the feet use multiple therapeutic elements:
- Deep heel cups improve stability
- Extended medial flanges control pronation
- Forefoot extensions offload painful joints
At PrimeCare, we’re proud to utilize advanced materials in our arthritis orthotics to provide optimal arthritis pain relief.
Our Tips on How to Prevent Arthritis

While genetic predisposition is out of your control, evidence-based prevention strategies significantly reduce arthritis risk and slow progression in the early stages.
Maintain optimal body weight through balanced nutrition, emphasizing anti-inflammatory foods. For example, Mediterranean diets rich in olive oil, fish, and vegetables show protective effects. Regular low-impact exercise like swimming or cycling builds supporting muscle while avoiding joint trauma.
Workplace modifications include:
- Ergonomic assessments to prevent repetitive strain
- Proper lifting techniques to protect the spine and knees
- Regular position changes to avoid sustained stress
- Supportive footwear to reduce impact forces
Address injuries promptly through appropriate rehabilitation, preventing post-traumatic arthritis. Smoking cessation reduces RA risk while improving overall joint health.

.svg)
.svg)



