At PrimeCare, Critical limb ischemia receives focused attention because of its serious impact on circulation, mobility, and limb health. Care pathways guide treatment for advanced vascular conditions, helping meet both medical and prosthetic needs to preserve limbs and support recovery.
Defining Critical Limb Ischemia
Critical limb ischemia is the end-stage manifestation of peripheral arterial obstruction. It’s defined clinically by the presence of ischemic rest pain, non-healing ulcers, or gangrene attributable to objectively proven arterial occlusive disease. While peripheral artery disease (PAD) is common, CLI is the point at which the circulatory system can no longer meet the basic metabolic demands of the tissue at rest.
Signs and Visible Symptoms of Critical Limb Ischemia
The symptoms of this condition are distinct and progressive. Identifying these signs early is essential for limb salvage.
- Ischemic rest pain: A burning or aching sensation in the feet or toes that intensifies at night.
- Non-healing wounds: Minor cuts or sores on the feet and legs that do not show signs of healing over several weeks.
- Skin changes: The skin on the affected limb often appears shiny, smooth, dry, or unusually pale.
- Tissue necrosis: The development of gangrene, where skin and underlying tissue turn black and die due to a total lack of blood supply.
- Pulse absence: A medical examination often reveals a weak or completely absent pulse in the groin, behind the knee, or at the ankle.
Across New Mexico, individuals with these signs often need coordinated vascular and mobility-focused care as the condition advances.

How Common Is Critical Limb Ischemia?
Critical limb ischemia affects a smaller proportion of individuals with peripheral arterial disease, yet it carries a disproportionate clinical burden due to high rates of complications, hospitalization, and mortality.
Epidemiological insights include:
- Approximately 1-2 percent prevalence among adults over 50, representing the most advanced stage of peripheral arterial disease.
- Higher incidence among diabetic populations, where vascular damage and neuropathy accelerate disease progression.
- Frequent hospitalizations, with studies showing that a significant proportion of patients need readmission within six months due to wound complications, infection, or recurrent ischemia.
- Elevated amputation risk within the first year, with major limb loss occurring at notably higher rates compared to earlier stages of vascular disease.
Healthcare systems often manage this condition due to its complexity, poor long-term prognosis, and the need for coordinated vascular, surgical, and rehabilitative care.
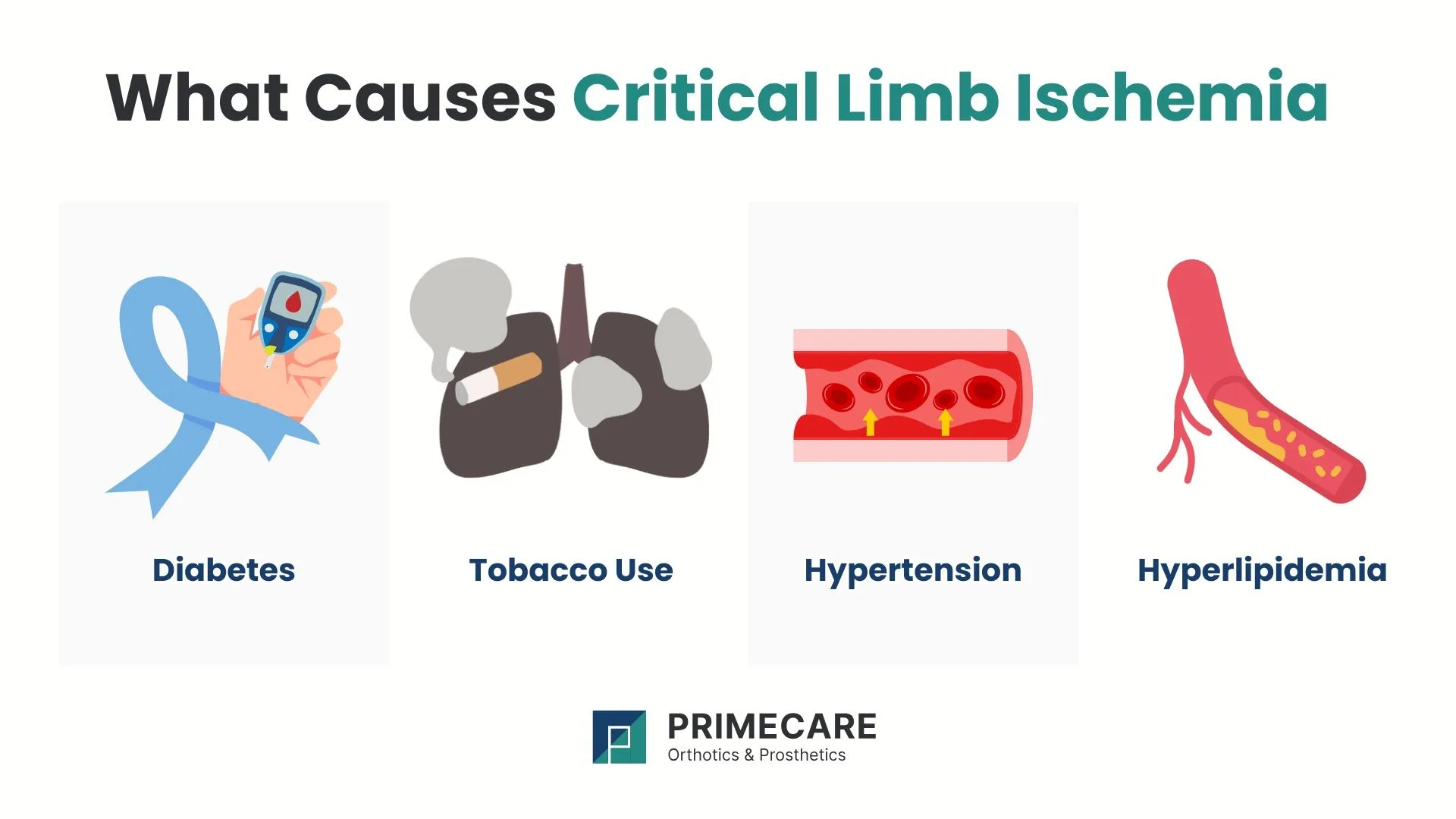
Critical Limb Ischemia Causes and Contributing Factors
Atherosclerosis is the primary driver for most cases. However, certain systemic factors accelerate the degradation of the arterial walls.
- Diabetes: Elevated blood sugar levels damage the lining of the blood vessels and the nerves.
- Tobacco use: Smoking remains the most significant modifiable risk factor.
- Hypertension: Chronic high blood pressure weakens the arteries’ structural integrity.
- Hyperlipidemia: High cholesterol levels contribute directly to plaque buildup.
These factors often coexist, compounding vascular damage and raising the risk of tissue loss.
Diagnostic Procedures for Critical Limb Ischemia
For an accurate diagnosis, doctors will use a physical examination and advanced imaging technologies to locate the exact site of the blockage.
- Ankle-brachial index (ABI): A comparison of blood pressure measured at the ankle and the arm.
- Doppler ultrasound: This non-invasive test uses sound waves to visualize blood flow through the vessels.
- CT angiography (CTA): A detailed scan that provides 3D images of the blood vessels using contrast dye.
- Magnetic resonance angiography (MRA): This utilizes magnetic fields to produce high-resolution images of the arterial structure.
Diagnostic findings shape both medical and post-surgical planning. For patients in New Mexico who experience limb loss or long-term mobility limitations following vascular intervention, PrimeCare provides tailored prosthetic care based on clinical evaluation, amputation level, and daily activity needs.
Treatment Options That Aim for Limb Preservation

The main treatment goal is to restore blood flow to prevent amputation. When salvage isn’t possible, the focus shifts to advanced mobility solutions.
1. Prosthetic Rehabilitation of Critical Limb Ischemia
In cases where tissue death is irreversible or infection poses a systemic threat, amputation becomes necessary. Following surgery, the restoration of independence relies on prosthetic technology:
- Below-the-knee (transtibial) prosthetics: These devices replace the leg from the mid-calf down, while the natural knee joint remains.
- Knee disarticulation prosthetics: These utilize the intact femur bone for weight-bearing after an amputation through the knee joint.
- Foot and partial foot prosthetics: These range from simple shoe inserts to custom-molded silicone restorations.
- Cosmetic covers: These flexible surfaces mimic the appearance of a natural limb to protect internal components.
PrimeCare proudly delivers these prosthetic services throughout New Mexico, offering device selection and fitting based on clinical evaluation and daily activity requirements.
2. Orthotic Braces and Support
For patients who retain their limb but suffer from muscle weakness or chronic wounds, orthotic intervention provides mechanical support.
- Ankle-foot orthoses (AFO): These braces stabilize the ankle and help with "foot drop", a common complication of nerve damage.
- Offloading braces: Specialized orthotics redistribute pressure away from ischemic ulcers on the bottom of the foot.
3. Endovascular Techniques for Critical Limb Ischemia
These minimally invasive procedures involve the use of catheters inserted through a small puncture in the groin.
- Angioplasty: A small balloon is inflated inside the artery to widen the narrowed segment.
- Stenting: A mesh tube is placed at the site of the blockage to keep the vessel open.
- Atherectomy: Specialized blades or lasers remove the plaque directly from the arterial wall.
4. Surgical Bypass
When arterial blockages cannot be treated with endovascular repair, surgeons reroute blood flow around the blockage using a vein from the patient or a synthetic graft to supply the lower leg or foot.
When Surgery and Amputation Become Necessary

Amputation in cases of critical limb ischemia becomes a medical necessity when profound blood flow obstruction leads to irreversible tissue decay. This clinical decision follows a rigorous evaluation after revascularization options cannot restore adequate circulation.
Amputation may be required due to:
- Tissue death: Irreversible loss of cellular function in the muscles or skin.
- Progressive gangrene: The spread of necrotic tissue that threatens the health of the entire limb.
- Severe infection: Deep-seated bacterial growth that risks systemic sepsis.
- Non-healing ulcers: Open wounds that remain unresponsive to wound care and vascular repair.
- Persistent ischemic pain: Chronic, intractable pain that diminishes the patient’s quality of life.
The specific level of removal depends on the extent of healthy tissue and local circulation. Procedures include partial foot, below-knee, or above-knee removal. Preserving natural joints supports improved mobility and more efficient prosthetic use.
Long-Term Outlook of Critical Limb Ischemia
Outcomes for critical limb ischemia vary based on the timing of treatment and overall health status.
Positive indicators include:
- Successful revascularization
- Controlled cardiovascular risk factors
- Adherence to medical therapy
Long-term care considerations involve:
- Ongoing vascular monitoring
- Lifestyle modification support
- Prosthetic adaptation and rehabilitation
With the right care pathways, many individuals regain mobility and maintain their independence.

.svg)
.svg)



