At PrimeCare, we understand the unique challenges that individuals with Muscular Dystrophy (MD) and their families face. Our specialized team combines cutting-edge orthotic technology with compassionate care, designing adaptive solutions that evolve with each patient's changing needs. Our devices help maintain independence and quality of life throughout their journey.
What Is Muscular Dystrophy?
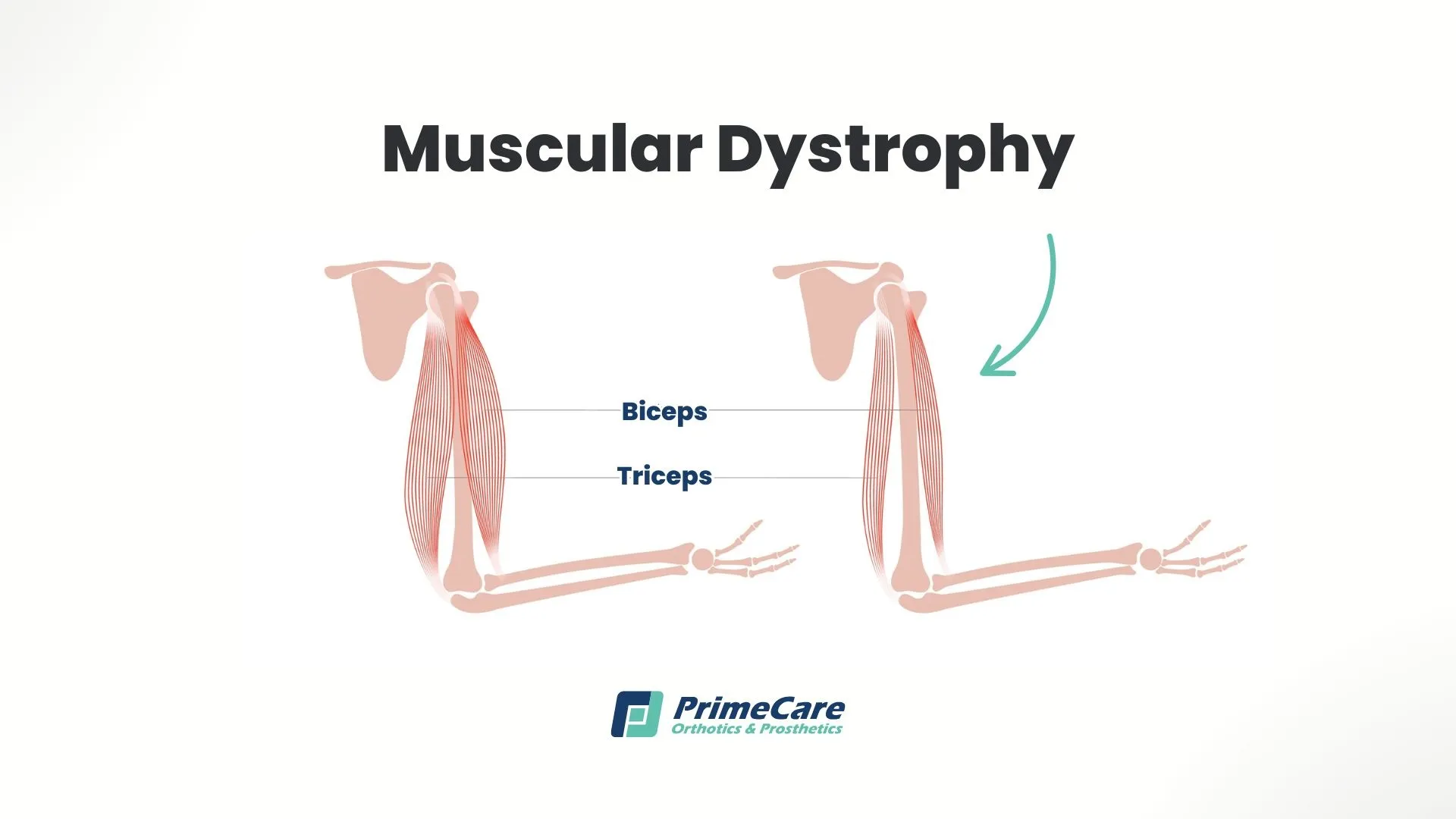
Muscular dystrophy encompasses over 30 genetic conditions characterized by progressive muscle weakness and degeneration. These disorders result from mutations in genes responsible for producing proteins essential for healthy muscle function, particularly dystrophin.
Without these crucial proteins, muscle fibers gradually break down faster than the body can repair them, leading to increasing weakness. The progression varies dramatically between types; some manifest in early childhood, while others don't appear until adulthood. Each form of muscular dystrophy presents unique challenges needing individualized treatment approaches and orthotic interventions.
Major Types of Muscular Dystrophy
We’ve outlined the distinct characteristics of each MD type to help determine appropriate orthotic interventions:
Duchenne Muscular Dystrophy (DMD)
The most severe childhood form is DMD, and it typically manifests at ages 2-5 in boys. Progressive weakness begins in the hips and pelvis, spreading to the shoulders, arms, and legs. Without intervention, most children require wheelchair use by age 12.
Becker Muscular Dystrophy (BMD)
This is a milder variant with similar symptoms to Duchenne but slower progression. Onset occurs between ages 5–60, typically during the teenage years, with many maintaining ambulation into their 30s or 40s.
Myotonic Dystrophy
The most common adult-onset form is myotonic dystrophy. It’s characterized by prolonged muscle contractions and the inability to relax muscles after use. Myotonic dystrophy affects multiple body systems, including the heart and lungs.
Congenital Muscular Dystrophies (CMD)
Present from birth, these forms vary widely in severity. Some progress slowly with mild disability, while others advance rapidly, causing serious complications.
Additional Types
- Limb-girdle MD: Primarily affects the hip and shoulder muscles.
- Facioscapulohumeral MD: Begins in the facial, shoulder, and upper arm muscles.
- Emery-dreifuss MD: Notable for early joint contractures and cardiac involvement.
- Oculopharyngeal MD: Affects eyelids and throat muscles, typically after age 40.
How Common Is Muscular Dystrophy?
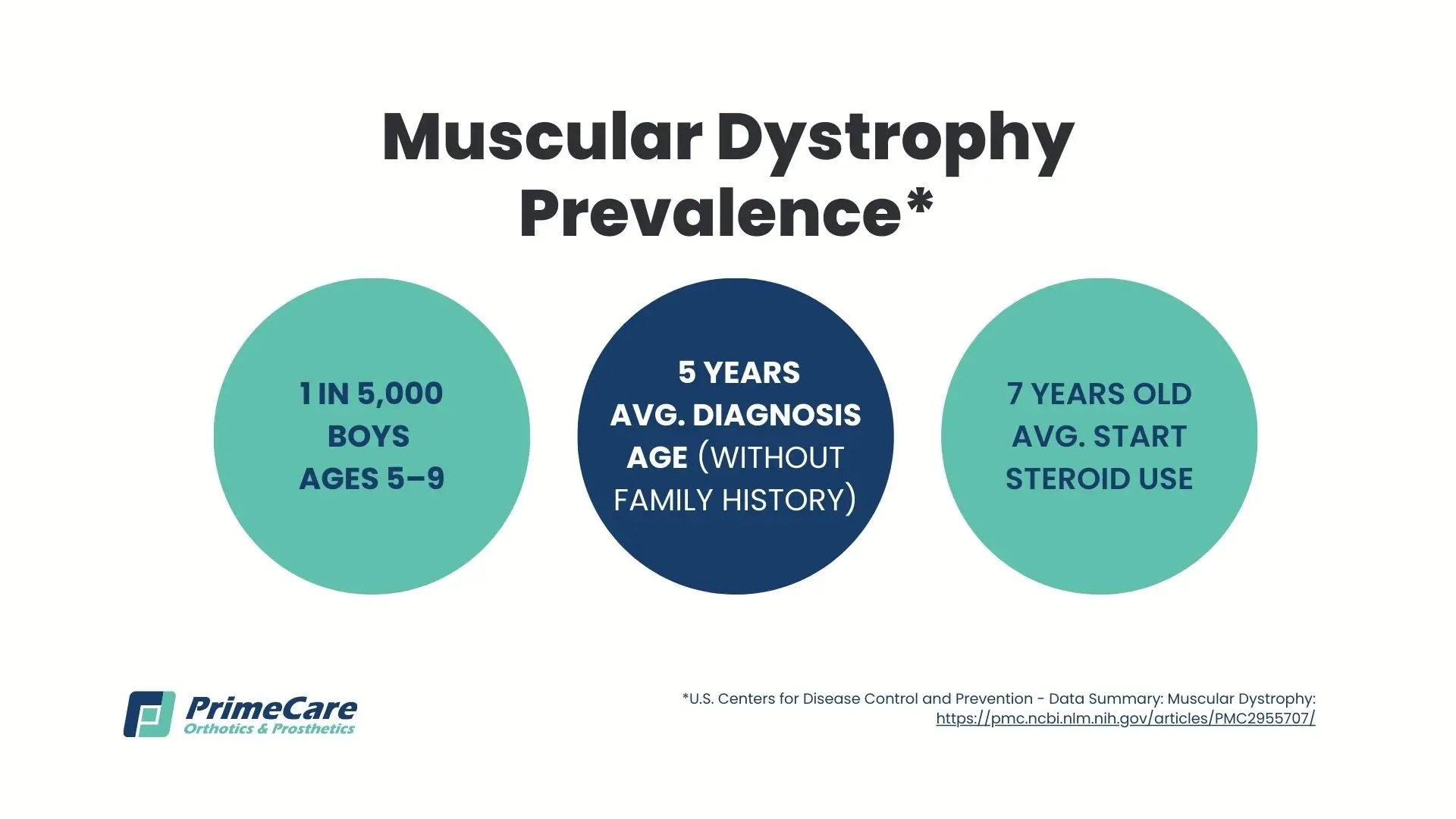
Muscular dystrophy affects approximately 16-25 per 100,000 people in the United States. The most prevalent forms include:
- Duchenne MD: Affects 1 in 3,500-5,000 male births globally.
- Myotonic dystrophy: Most common adult form, affecting 1 in 8,000 individuals worldwide.
- Facioscapulohumeral MD: Impacts approximately 4 in 100,000 people.
- Limb-girdle MD: Occurs in 2 per 100,000 individuals.
The Muscular Dystrophy Association reports that over 250,000 Americans currently live with various forms of MD, with gender distribution varying by type; X-linked forms predominantly affect males, while autosomal types impact both genders equally.
Recognizing Early Signs of Muscular Dystrophy
The ability to recognize symptoms early allows for timely orthotic intervention and can significantly impact long-term outcomes. The manifestations of muscular dystrophy vary between types, but there are common patterns that progressively worsen over time. Parents often first notice subtle changes in their child's movement, while adults may experience unexplained muscle weakness or fatigue. Here are the common early symptoms:
- Frequent falls without apparent cause — more than typical childhood stumbles
- Difficulty rising from the floor using Gowers' sign (hands on thighs to "walk up" body)
- Trouble climbing stairs, running, or jumping
- Waddling gait pattern from hip muscle weakness
- Walking on toes or balls of feet due to heel cord tightness
- Progressive muscle weakness starting in the hips and shoulders
- Enlarged calf muscles (pseudohypertrophy) in DMD/BMD—looks like strength but is actually fat/fibrous tissue
- Muscle stiffness and pain, especially after rest
- Joint contractures developing gradually in the ankles, knees, and hips
- Spinal curvature (scoliosis) occurs as trunk muscles weaken
- Delayed motor milestones - late walking, inability to run or jump
- Breathing difficulties from respiratory muscle weakness
- Heart problems, including irregular rhythm and cardiomyopathy
- Swallowing difficulties increasing aspiration risk
- Learning disabilities or cognitive challenges in some types (especially Duchenne)
Risk Factors for Developing Muscular Dystrophy

Several factors influence the risk of developing MD:
- Family history: Primary risk factor for all inherited forms.
- Gender: Males face a higher risk for X-linked types (Duchenne, Becker).
- Genetic carrier status: Female carriers may have mild symptoms.
- Ethnicity: Certain populations show higher carrier frequencies.
- Parental age: Advanced maternal age slightly increases the risk of de novo mutations.
While environmental factors don't cause MD, they may influence progression. To preserve function longer, it’s important to maintain optimal health through proper nutrition, appropriate exercise, and avoiding obesity.
Potential Complications of Muscular Dystrophy
As muscle weakness progresses, it can lead to multiple complications requiring comprehensive management:
- Mobility limitations: Eventually requiring orthotic devices for muscular dystrophy, wheelchairs, or other adaptive equipment.
- Contractures: Shortened muscles and tendons limiting joint motion.
- Respiratory compromise: Weakened breathing muscles, increasing pneumonia risk.
- Cardiac involvement: Heart muscle weakness and rhythm abnormalities.
- Spinal deformity: Progressive scoliosis affecting posture and breathing.
- Nutritional challenges: Swallowing difficulties impacting adequate nutrition.
- Bone health: Reduced bone density from decreased weight-bearing activity.
A Comprehensive Diagnostic Approach to Muscular Dystrophy
The diagnostic journey typically starts when parents notice subtle changes in their child's movement patterns or when adults experience unexplained muscle weakness.
Initial Evaluation
The process starts with a detailed medical and family history, exploring symptom onset, progression patterns, and any relatives with similar conditions. Physical and neurological examinations assess muscle strength, reflexes, and coordination. Healthcare providers carefully observe movement patterns, notably how patients rise from the floor, climb stairs, and walk, looking for characteristic signs like the Gowers' maneuver or waddling gait.
Laboratory Testing
Next come lab tests. Blood tests measuring creatine kinase (CK) levels often provide the first objective evidence of muscle damage, with levels typically elevated 50-100 times normal in Duchenne MD. Genetic testing has revolutionized the diagnosis of MD, using techniques like multiplex ligation-dependent probe amplification to detect large deletions and next-generation sequencing to identify point mutations.
When genetic tests are inconclusive, electromyography (EMG) measures muscle electrical activity to distinguish myopathic from neuropathic conditions, while a muscle biopsy with immunohistochemical staining can reveal absent or reduced dystrophin and other muscle proteins.
Additional Assessments
A comprehensive evaluation includes cardiac assessment through ECG and echocardiogram to establish baseline heart function, as cardiac involvement may precede skeletal muscle symptoms in some types of MD.
Pulmonary function testing measures respiratory muscle strength and establishes the baseline values for monitoring progression. MRI provides detailed muscle imaging to assess fatty infiltration patterns, while developmental assessments help identify cognitive or behavioral challenges in children who are affected.
Modern Treatment Strategies for Muscular Dystrophy

Unfortunately, there’s no cure for MD. However, contemporary management embraces a proactive, multidisciplinary approach that targets multiple aspects of the disease simultaneously.
Medical Management
Corticosteroid therapy with prednisone or deflazacort continues to be the gold standard for Duchenne MD, proven to prolong ambulation by 2-5 years when initiated between ages 4-6. These medications work through multiple mechanisms, including reducing inflammation, stabilizing muscle membranes, and potentially upregulating compensatory proteins.
Revolutionary genetic therapies are transforming treatment possibilities, with exon-skipping drugs like eteplirsen and golodirsen enabling the production of shortened but partially functional dystrophin in patients with specific mutations.
Gene therapy trials using adeno-associated viral vectors are showing promising early results, though immune responses and delivery challenges are still significant hurdles. Cardiac medications protect heart function, while respiratory support addresses breathing difficulties as they develop.
Physical and Occupational Therapy
Regular therapy sessions help maintain flexibility and prevent contractures through daily stretching programs targeting heel cords, hip flexors, and iliotibial bands. Strengthening exercises are also helpful, but they must be carefully prescribed to preserve function without causing overwork damage to fragile muscle fibers.
Aquatic therapy is low-impact conditioning, while the buoyancy reduces stress on weakened muscles. Therapists also train patients and families in using adaptive equipment, from simple aids like reachers and dressing sticks to complex power mobility systems, depending on the individual’s needs.
Surgical Interventions
If surgery is needed, it should be timed carefully to maximize benefits while minimizing risks. Tendon lengthening procedures may address severe contractures limiting function, though overlengthening must be avoided to preserve remaining strength.
Spinal fusion for progressive scoliosis typically occurs when curves exceed 40-50 degrees and respiratory function is adequate. For patients with severe dysphagia, placing a feeding tube ensures adequate nutrition while reducing aspiration risk.
Nutritional Support
As MD progresses, it’s harder to maintain optimal nutrition. Early stages may require increased calories due to hyperactivity, while later stages predispose to obesity from reduced mobility. Dietitians are a great resource as they help balance macronutrient intake while ensuring adequate calcium and vitamin D for bone health, protein for muscle maintenance, and appropriate caloric intake to prevent both malnutrition and excessive weight gain.
Specialized Orthotic Solutions for Muscular Dystrophy

At PrimeCare, we’re proud to provide comprehensive orthotic devices tailored to each patient's specific needs and evolving disease stage.
Ankle-Foot Orthoses (AFO)
Our AFO muscular dystrophy devices address the spectrum of lower leg weakness patterns seen in MD patients. For minimal weakness, flexible leaf-spring designs provide just enough support to clear the foot during the swing phase while allowing some ankle motion. As weakness progresses, solid AFOs offer maximum support for significant foot drop, maintaining the ankle in optimal position throughout the gait cycle.
Ground reaction AFOs extend higher on the leg to improve knee stability when quadriceps weakness develops, while dynamic AFOs incorporate energy-storing materials that assist with push-off in more active patients.
At PrimeCare, all of our custom AFOs utilize lightweight materials like carbon fiber and advanced thermoplastics, with features specifically designed for MD patients, including accommodative linings for sensitive skin and growth adjustability for pediatric users.
Knee-Ankle-Foot Orthoses (KAFO)
As proximal weakness advances, our KAFOs provide comprehensive support while maximizing remaining function. Stance-control technology is a significant advancement, with sophisticated joints that lock during weight-bearing for stability, then automatically unlock during the swing phase to allow for more natural gait patterns than traditional locked-knee designs.
Carbon fiber construction minimizes weight, a crucial factor for patients with limited strength reserves. Custom alignment addresses individual gait deviations, while growth-adjustable features in pediatric designs reduce replacement frequency as children develop.
Spinal Bracing Solutions
Progressive scoliosis affects up to 90 percent of non-ambulatory MD patients, requiring specialized intervention. Our custom-molded TLSOs (thoracolumbosacral orthoses) provide three-point pressure correction to slow curve progression while accommodating respiratory needs through flexible anterior sections.
The lightweight thermoplastic construction allows patients to wear the brace all day comfortably, while strategic padding prevents skin breakdown. For wheelchair users, we integrate spinal orthoses with seating systems to provide comprehensive postural support throughout daily activities.
Dynamic Lycra Garments
Compression garments are a less restrictive alternative or complement to rigid bracing. Custom-fitted suits provide proprioceptive input that enhances body awareness and postural control. Strategic reinforcement panels offer additional support where needed without restricting movement. The breathable, moisture-wicking materials ensure comfort during extended wear, while the discreet design allows patients to wear these garments under regular clothing in school or work settings.
Custom Foot Orthotics
Specialized insoles address the unique foot changes seen in MD patients. Accommodative materials like plastazote prevent pressure sores in areas of bony prominence, while biomechanical corrections optimize alignment within the kinetic chain. Strategic cushioning reduces impact forces on weakened muscles and joints. For patients using AFOs, we design orthotics that integrate seamlessly, providing comprehensive lower limb support from foot to knee.
Prevention Strategies and Genetic Counseling for Muscular Dystrophy

While it’s impossible to prevent inherited muscular dystrophy, comprehensive genetic counseling empowers informed family planning:
- Carrier testing identifies at-risk family members
- Prenatal diagnosis via CVS or amniocentesis
- Preimplantation genetic diagnosis with IVF
- Genetic counseling for risk assessment
For affected individuals, proactive health maintenance is essential, such as appropriate exercise, prompt infection treatment, optimal nutrition, and early orthotic intervention before contractures develop.

.svg)
.svg)



