At PrimeCare, we understand that living with cervical spondylosis can significantly impact your daily life. Our expert orthotic team specializes in providing personalized neck support solutions that address the unique challenges of this degenerative condition to help minimize your pain.
What Is Cervical Spondylosis?
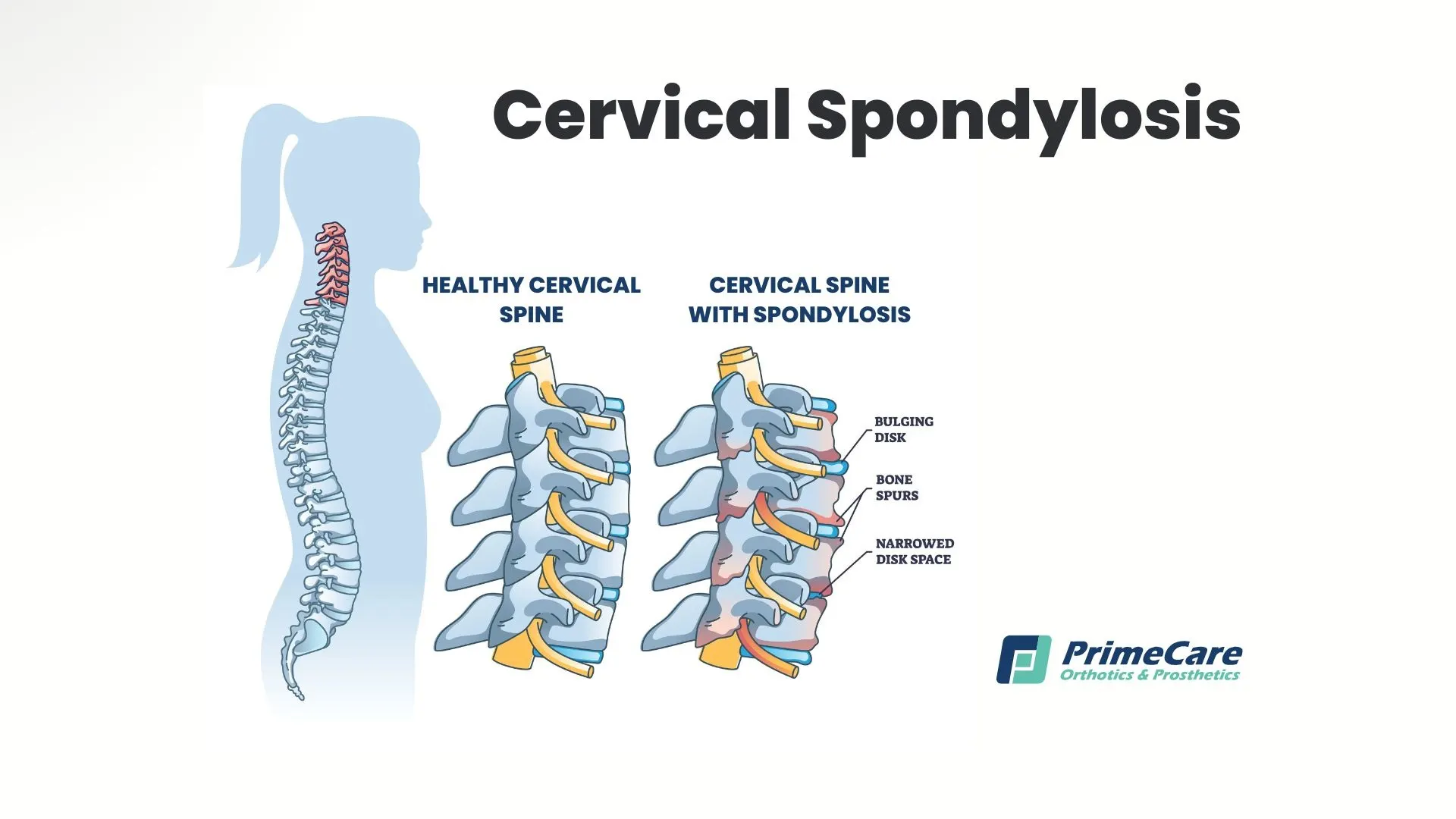
Cervical spondylosis, also known as cervical osteoarthritis or neck arthritis, is an age-related condition affecting the cervical spine. This degenerative disorder occurs when the disks and joints in your neck undergo wear and tear, leading to changes in the bones, disks, and ligaments.
As the spinal disks lose hydration and shrink, bone spurs may develop and potentially compress spinal nerves, resulting in various symptoms. The condition primarily affects the seven vertebrae in your neck (C1–C7) and the soft tissues between them, progressively altering the spine's structure and function over time.
How Common Is Cervical Spondylosis?
This condition is remarkably prevalent, affecting more than 85% of people over age 60. Studies show that cervical degeneration begins as early as the 30s, with the majority experiencing some degree of cervical spine changes by middle age. Despite its prevalence, many individuals remain asymptomatic, making it one of the most common yet underdiagnosed neck conditions.
Signs and Symptoms

Cervical spondylosis manifests through various symptoms that can range from mild discomfort to severe impairment:
- Neck pain that may radiate to the shoulders and arms
- Stiffness limiting neck movement, especially in the morning
- Grinding or popping sensations during head rotation
- Headaches originating from the base of the neck
- Muscle weakness in arms or hands
- Numbness or tingling in extremities
- Balance difficulties or unsteady gait
- In severe cases, bladder or bowel control issues
These symptoms often worsen with movement and may fluctuate in intensity throughout the day.
Causes of Cervical Spondylosis
The main cause is natural aging, but several factors accelerate the degenerative process:
- Disk dehydration: Spinal disks lose fluid content, reducing their cushioning ability.
- Herniated disks: Cracks in disk exteriors allow soft inner material to protrude.
- Bone spurs: Extra bone growth attempts to strengthen the weakened spine.
- Ligament stiffening: Connective tissues lose flexibility and reduce the range of motion.
Risk Factors

The better you understand risk factors, the easier it is to intervene early and implement prevention strategies:
- Age: Primary risk factor, with incidence increasing significantly after 40.
- Occupational hazards: Jobs requiring repetitive neck movements, overhead work, or prolonged computer use.
- Previous neck injury: History of whiplash injuries, automobile accidents, or trauma.
- Genetic predisposition: Family history of spine problems.
- Lifestyle factors:
- Smoking, which accelerates disk degeneration.
- Poor posture during daily activities.
- Lack of regular exercise.
- Carrying heavy loads improperly.
- Gender: Slightly more common in men.
- Chronic conditions: Obesity, diabetes, and inflammatory disorders.
These factors often compound and create a higher risk profile for developing severe neck pain and complications.
Cervical Spondylosis Complications
While many cases remain manageable, untreated cervical spondylosis can lead to serious complications that impact quality of life. Cervical radiculopathy occurs when bone spurs or herniated disks compress nerve roots, causing arm pain and weakness. More severe compression of the spinal canal can result in cervical myelopathy, potentially causing permanent nerve damage, coordination problems, and bladder dysfunction.
How Is Cervical Spondylosis Diagnosed?

Accurate diagnosis involves comprehensive evaluation by a healthcare provider:
- Physical examination: Assessment of neck movement, reflexes, and muscle strength.
- Imaging studies:
- X-rays reveal bone spurs and disk space narrowing.
- MRI shows soft tissue details, nerve compression, and spinal cord involvement.
- CT scans provide detailed bone structure images.
- Neurological tests: Electromyography (EMG) evaluates nerve function.
- Clinical history: Discussion of symptoms, previous injuries, and occupational factors.
Early diagnosis allows for prompt treatment, making it easier to prevent progression and lessening the need for invasive interventions.
How Is Cervical Spondylosis Treated?
Treatment approaches vary based on severity, ranging from conservative management to surgical intervention:
Physical Therapy
A skilled physical therapist serves as your partner in recovery, developing individualized exercise programs that target the specific challenges of cervical spondylosis. The therapeutic approach begins with gentle stretching exercises designed to gradually increase your cervical range of motion without causing additional strain.
As flexibility improves, strengthening routines focus on the deep neck muscles and surrounding shoulder girdle, creating a natural support system for your cervical spine. Posture correction training addresses the biomechanical factors contributing to your condition, teaching you how to maintain proper alignment during daily activities. Manual therapy techniques, such as gentle mobilization and soft tissue work, help alleviate pain while improving joint function and reducing muscle tension.
Medication Management
Effective pain management often requires a strategic approach to using medication. For mild symptoms, over-the-counter pain relievers provide adequate relief, particularly when combined with other conservative treatments. Anti-inflammatory medications help reduce swelling around compressed nerves and irritated joints, addressing both pain and the underlying inflammation.
When muscle spasms contribute to discomfort, muscle relaxants offer targeted relief. The result is better sleep and improved participation in physical therapy. When neck pain is severe or persistent, healthcare providers may prescribe stronger medications, carefully balancing pain relief with potential side effects to ensure optimal patient outcomes.
Injection Therapies

Epidural steroid injections deliver powerful anti-inflammatory medication directly to compressed nerve roots, often providing weeks to months of significant pain relief. This targeted approach reduces the need for systemic medication while maximizing therapeutic benefit at the pathology site.
Facet joint injections address the arthritic changes common in cervical spondylosis, using a combination of anesthetic and steroid to calm inflamed joint capsules. For patients experiencing painful muscle spasms secondary to their condition, trigger point injections help break the pain-spasm cycle, allowing for more effective participation in physical therapy and exercise programs.
Alternative Therapies
Acupuncture has shown promising results for chronic pain management, with studies suggesting it may help reduce inflammation and promote natural pain-relieving mechanisms. When experienced practitioners familiar with cervical spondylosis perform chiropractic care, it can help restore proper joint mechanics through gentle adjustments.
Heat therapy increases blood flow and relaxes tense muscles, while cold applications reduce acute inflammation and numb painful areas. TENS (Transcutaneous Electrical Nerve Stimulation) units provide non-invasive pain control through electrical impulses that interfere with pain signal transmission, offering patients a drug-free option to manage symptoms.
Surgical Interventions
Surgery is reserved for severe cases where conservative treatment fails or when neurological compromise threatens permanent damage. Anterior cervical discectomy and fusion (ACDF) removes damaged disk material and bone spurs compressing neural structures, then stabilizes the spine through fusion of adjacent vertebrae. This procedure helps relieve nerve compression while eliminating painful motion at the affected level. Cervical laminectomy creates additional space within the spinal canal by removing portions of the lamina, relieving pressure on the spinal cord in cases of severe stenosis.
For younger patients who want to maintain mobility, artificial disk replacement is an alternative to fusion, preserving natural neck movement while addressing the underlying pathology. These surgical options aren’t right for everyone, and the risks and benefits should be discussed with experienced spine surgeons beforehand.
Lifestyle Modifications

Successful management requires comprehensive lifestyle changes:
- Ergonomic workplace adjustments
- Regular exercise focusing on neck and shoulder strength
- Weight management to reduce spinal stress
- Smoking cessation to slow degeneration
- Proper sleeping positions with appropriate pillow support
Specialized Cervical Spondylosis Braces
Neck braces play a key role in easing pain and supporting your recovery.
Types of Neck Braces for Cervical Spondylosis
At PrimeCare, we provide comprehensive neck bracing options tailored to each individual’s needs:
Soft cervical collars: Ideal for moderate neck pain and early-stage management:
- Made from comfortable foam materials
- Provide gentle support while allowing limited movement
- Perfect for temporary relief during acute flare-ups
- Recommended wearing time: 2–3 hours daily, not exceeding more than a week without medical supervision
Rigid cervical collars: Designed for severe cases requiring neck immobilization:
- Hard collars with adjustable chin supports
- Restrict neck movement to promote healing
- Essential after neck surgery or traumatic injury
- Custom-fitted to ensure proper alignment
Specialized bracing options:
- Foam cervical collars with moisture-wicking properties
- Adjustable neck support devices for gradual mobility restoration
- Night-specific braces using a thin pillow design
- Posture corrector integration for long-term benefits
How Neck Braces Work for Cervical Spondylosis
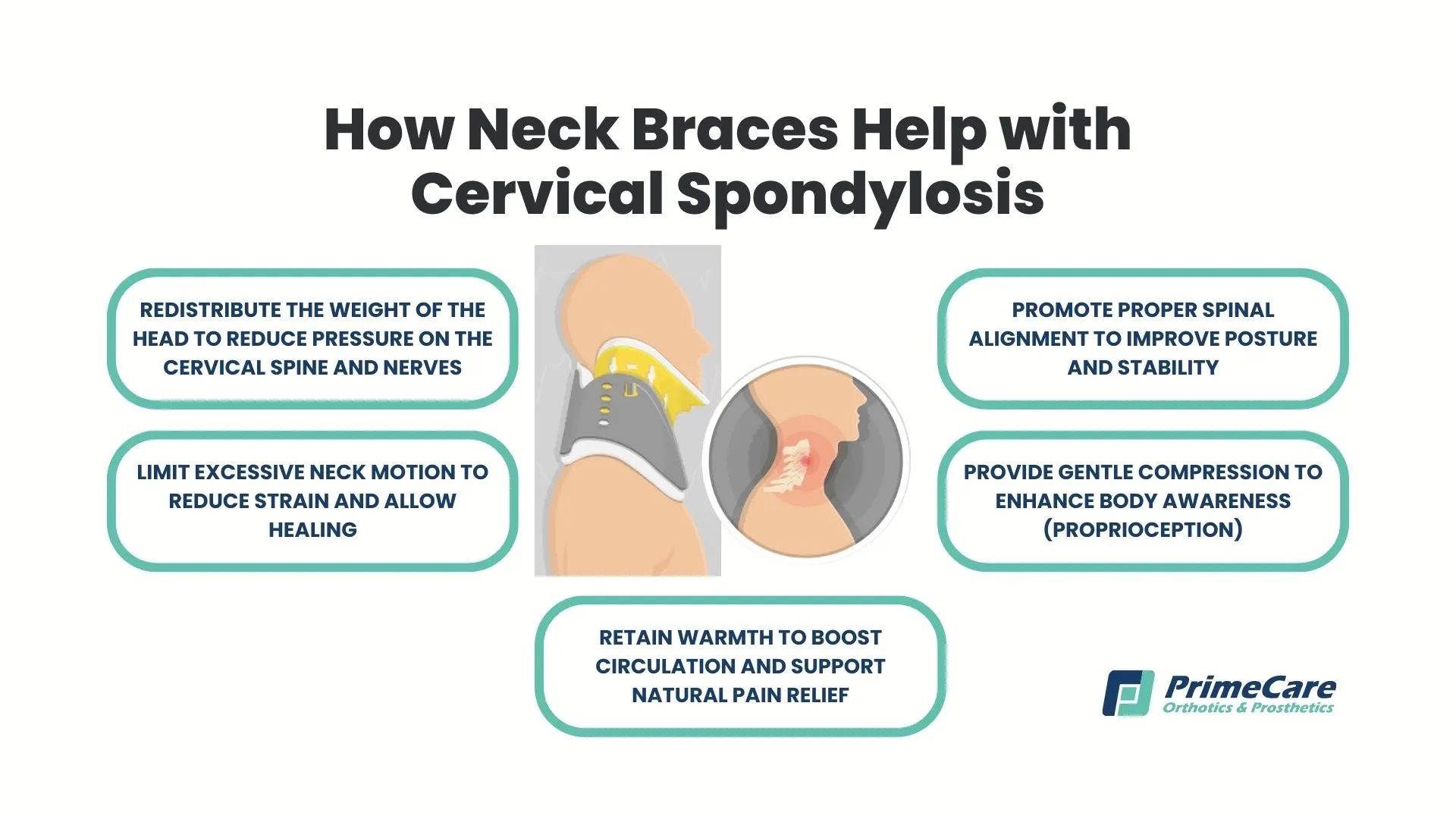
Cervical collars and neck braces function through multiple therapeutic mechanisms to provide relief and promote healing. These devices work by redistributing the weight of your head away from the affected cervical spine segments, reducing compression on damaged disks and irritated nerve roots. Braces limit neck movement and prevent repetitive strain on inflamed tissues while maintaining proper spinal alignment.
The gentle compression that well-fitted collars provide also enhances proprioception, your body's awareness of neck position, which helps retrain proper posture patterns. Additionally, the warmth that the brace material retains increases local blood flow, promoting the healing process and providing natural pain relief through improved circulation.
Guidelines for Using Braces Properly
Using a cervical brace correctly is important to ensure comfort, effectiveness, and safety. Follow these general guidelines:
- Always follow your healthcare provider’s recommendations
- Avoid continuous wear to prevent muscle weakening
- Ensure proper fit to reduce pressure points
- Clean regularly to prevent skin irritation
- Gradually reduce usage as symptoms improve

.svg)
.svg)