At PrimeCare, we recognize how even slight differences in leg length can affect your posture, gait, and overall quality of life. Our pedorthic specialists provide comprehensive assessments and custom orthotic solutions designed to restore balance and reduce discomfort associated with uneven leg lengths.
What Is Leg Length Discrepancy?
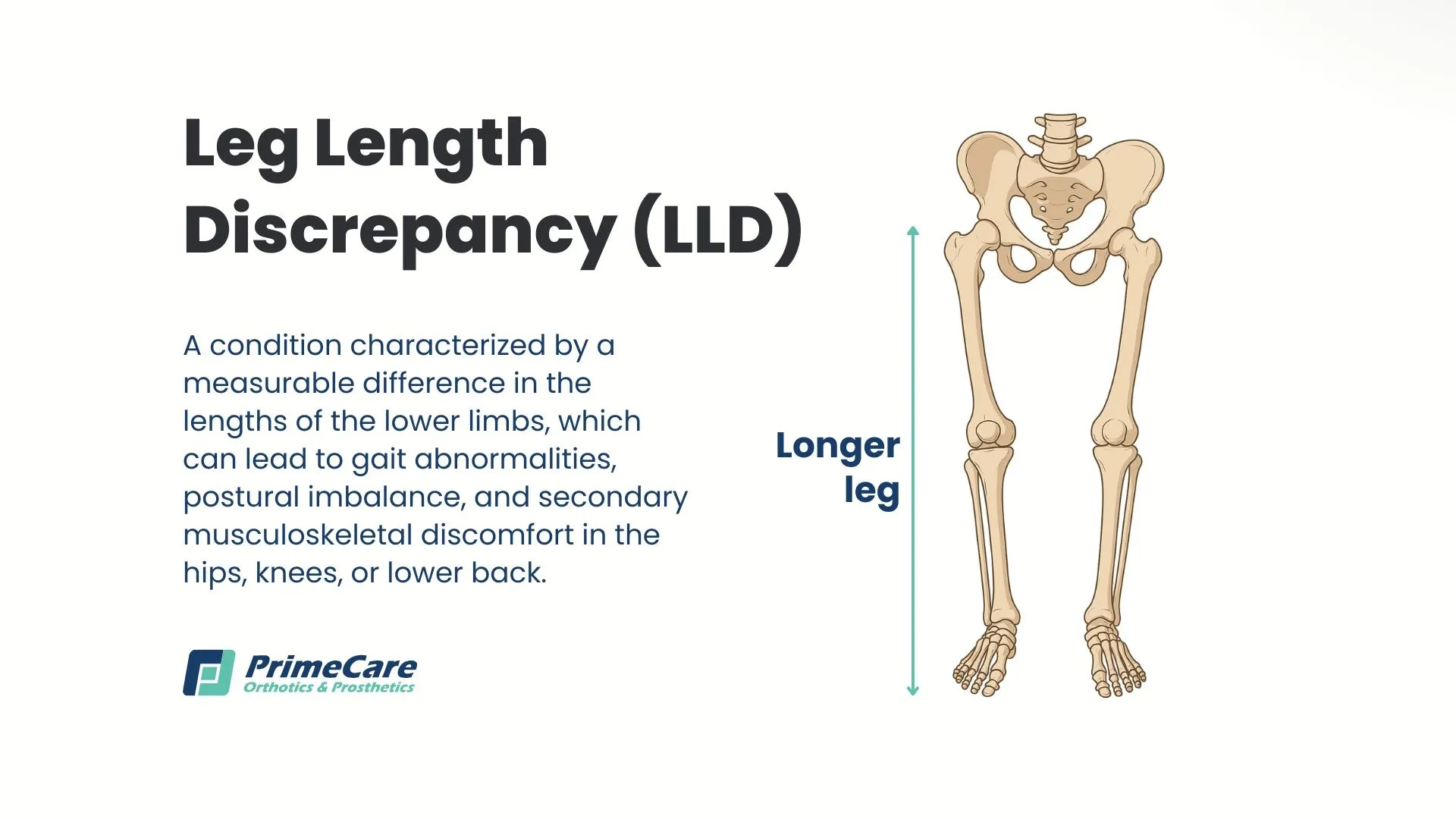
Leg length discrepancy (LLD), also called limb length inequality or anisomelia, is a condition where one leg is measurably shorter than the other, affecting the biomechanical alignment of the lower body. This inequality may involve the entire leg or specific segments, such as the femur (thigh bone) or tibia (shin bone). The difference ranges from barely noticeable to several centimeters, with varying effects on daily function and comfort.
The condition can develop during fetal development, appear during childhood growth, or result from injury or disease later in life. While many people have minor differences that cause no symptoms, larger discrepancies often lead to compensatory movement patterns that stress joints, muscles, and the spine over time.
How Common Is Leg Length Discrepancy?
You may be surprised to learn that leg length inequality is prevalent in the general population. Research indicates that between 40% and 70% of adults have some degree of leg length difference, with estimates suggesting up to 35% have a discrepancy of 0.5 to 1.5 centimeters. However, most people with minor differences (less than 5-10 millimeters) experience no symptoms and may never be aware that they have the condition.
Clinically significant leg length discrepancies, those causing symptoms or functional limitations, are less common but still affect a substantial number of individuals. The condition appears to occur equally across genders, though certain causes may be more prevalent in specific populations.
Types of Leg Length Discrepancy

Understanding whether your leg length difference is structural or functional is essential for determining the most effective treatment approach.
Structural Leg Length Discrepancy (Anatomical LLD)
Structural or anatomical leg length discrepancy occurs when there is an actual difference in the length of the bones themselves. One or both bones in the leg — the femur and/or tibia — measure shorter on one side compared to the other. This true shortening can be:
- Congenital: Present from birth due to developmental conditions like femoral deficiency, fibular hemimelia, or conditions such as hemiatrophy (underdevelopment of one side of the body) or hemihypertrophy (overgrowth of one side).
- Developmental: Resulting from growth plate disturbances, infections during childhood, or conditions like neurofibromatosis or Ollier disease that affect bone development.
- Acquired: Caused by trauma, improperly healed fractures, bone infections (osteomyelitis), tumors, or surgical procedures, including hip or knee replacement.
Structural discrepancies are typically permanent unless they’re corrected through surgical intervention. This makes accurate measurement critical for determining appropriate orthotic lift heights.
Functional Leg Length Discrepancy (Apparent LLD)
Functional or apparent leg length discrepancy occurs when the bones are equal in length, but muscular imbalances, joint restrictions, or alignment issues create the appearance and symptoms of unequal leg length. Here are some common causes:
- Pelvic obliquity: Tilting or rotation of the pelvis due to muscle tightness, particularly in the hip flexors or gluteal muscles.
- Scoliosis: Lateral curvature of the spine that creates asymmetry in the torso and pelvis.
- Joint contractures: Limited range of motion in the hip, knee, or ankle that prevents full extension.
- Asymmetrical foot mechanics: Excessive pronation (rolling inward) on one foot compared to the other, effectively shortening one leg during weight-bearing.
Functional discrepancies often respond well to physical therapy, chiropractic care, and temporary orthotic support while underlying musculoskeletal issues are addressed. Unlike structural LLD, functional discrepancies may resolve when the root cause is treated appropriately.
Signs and Symptoms of Leg Length Discrepancy
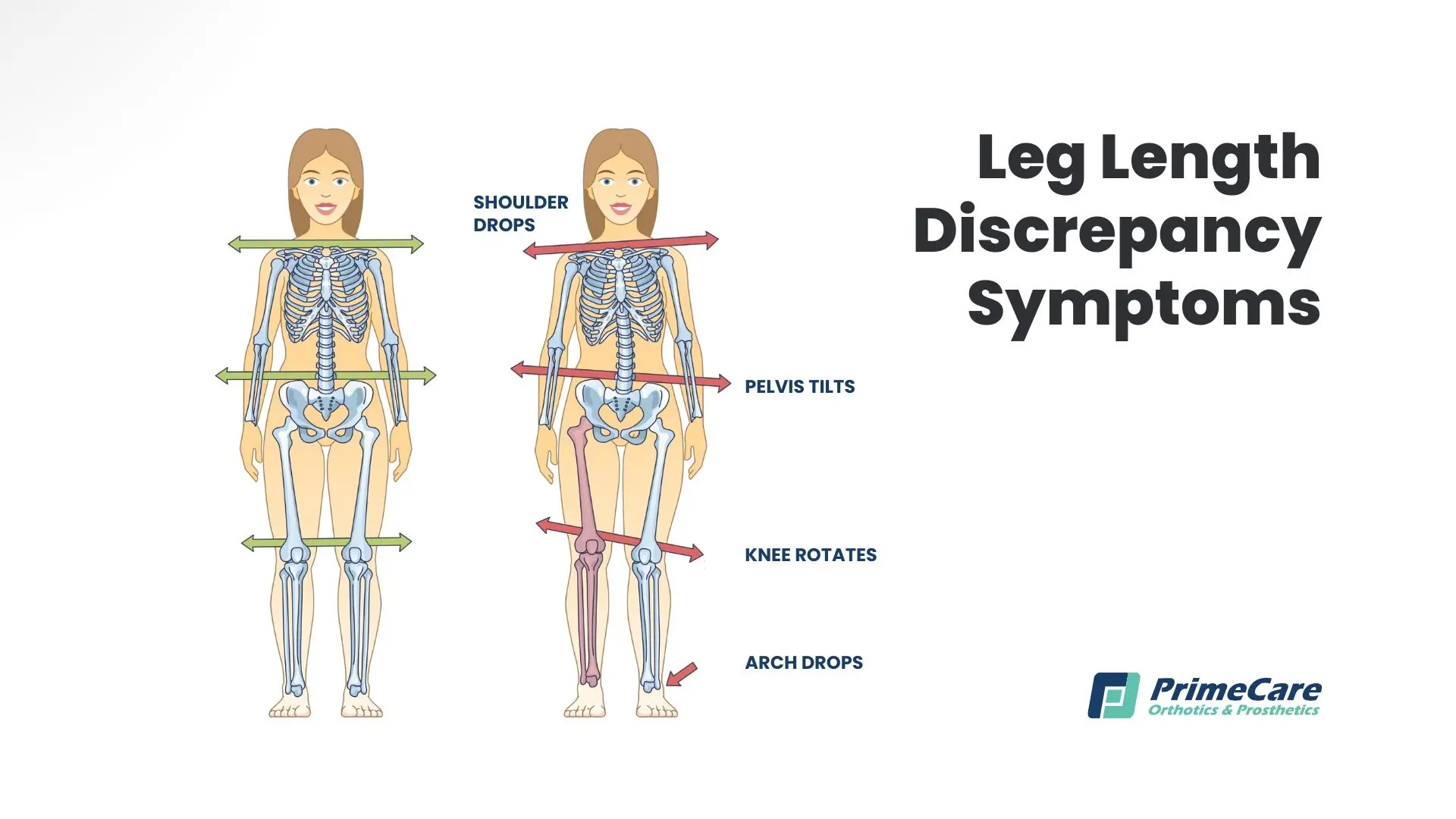
The symptoms of leg length inequality vary depending on the magnitude of the difference, whether it's structural or functional, and individual factors such as age and activity level. Smaller discrepancies typically produce milder symptoms or none at all.
Lower Body Symptoms
- Noticeable limping or altered gait pattern
- Walking on the toes or the ball of the shorter leg to compensate
- Knee pain, particularly in the longer leg, due to increased stress
- Hip pain or discomfort, especially in the hip of the shorter leg
- Ankle instability or recurrent ankle injuries
- Leg muscle fatigue or cramping after walking or standing
Spinal and Postural Symptoms
- Lower back pain, often chronic and persistent
- Pelvic tilting or asymmetry is visible when standing
- Scoliosis or lateral spinal curvature
- Shoulder height differences
- Neck pain or tension from compensatory head positioning
- General postural imbalance with a visible lean to one side
Functional Limitations
- Difficulty with balance, particularly during single-leg activities
- Reduced endurance during walking or prolonged standing
- Challenges with athletic activities requiring symmetrical movement
- Discomfort when bending, twisting, or performing activities that stress the lower back
- Frequent tripping or falling due to altered gait mechanics
Secondary Effects
- Premature wear and tear on joints (early onset osteoarthritis)
- Stress fractures in the longer leg from increased load
- Soft tissue overuse injuries, including plantar fasciitis, Achilles tendinitis, and iliotibial band syndrome
- Psychological impact on body image and self-esteem, particularly in visible cases
Causes of Leg Length Discrepancy

Leg length inequality develops through numerous pathways, ranging from congenital conditions to acquired injuries and diseases. Let’s examine the specifics.
Congenital and Developmental Causes
Conditions present at birth or developing during childhood growth include developmental dysplasia of the hip (DDH), where improper hip socket formation affects leg positioning; congenital femoral or tibial deficiencies, where bones form incompletely; hemiatrophy or hemihypertrophy causing asymmetric body growth; and overgrowth syndromes such as Beckwith-Wiedemann syndrome, Klippel-Trenaunay syndrome, and Proteus syndrome. Genetic skeletal dysplasias and conditions like neurofibromatosis type 1 can also disrupt normal bone growth patterns.
Traumatic Causes
Physical injuries affecting bone length include fractures that heal with the bone shortened or displaced; growth plate fractures (physeal fractures) that accelerate or slow bone growth; severe burns affecting bone development; and unsuccessful joint replacement surgeries that alter leg length. Radiation therapy received during childhood, while bones are still growing, can also impact final leg length.
Infectious and Inflammatory Causes
Infections and inflammatory conditions can significantly impact bone growth, including osteomyelitis (bone infection), septic arthritis (joint infection), tuberculosis affecting bone, juvenile idiopathic arthritis, and rheumatoid arthritis. These conditions may either stimulate excessive growth due to increased blood flow during active infection or inhibit growth via growth plate damage.
Neuromuscular Causes
Neurological conditions affecting muscle tone and bone development include cerebral palsy, which creates muscle imbalances that affect bone growth; polio, which can cause muscle weakness and bone undergrowth; and various muscular dystrophies impacting bone-muscle interaction.
Degenerative Causes
Ollier disease creates benign cartilage growths that disrupt normal bone elongation, while hereditary multiple osteochondromas (exostoses) produce bone tumors that can reduce growth potential. Avascular necrosis (bone death due to poor blood supply) and severe osteoarthritis with joint collapse can also create functional leg length differences.
Unfortunately, in many cases, particularly mild congenital discrepancies, the exact cause remains unknown despite thorough medical investigation.
Risk Factors for Developing Leg Length Discrepancy

Several factors increase the likelihood of developing clinically significant leg length inequality or experiencing symptoms from existing discrepancies:
Demographic and lifestyle factors:
- Older age when undergoing hip or knee replacement surgery, as tissue adaptation becomes more difficult.
- Being overweight or obese, which increases stress on already asymmetric joints and accelerates compensatory wear patterns.
- Occupations requiring prolonged standing, repetitive single-leg loading, or heavy lifting that magnify the effects of even minor discrepancies;
- High-impact sports participation, particularly running sports, where repetitive impact multiplies biomechanical stresses.
- Sedentary lifestyle with weak core and hip stabilizer muscles, reducing the body's ability to compensate effectively.
Medical and treatment history:
- Delayed diagnosis or treatment of childhood orthopedic conditions, allowing discrepancies to progress unchecked.
- Previous unilateral (one-sided) orthopedic surgeries that may alter bone length or joint positioning.
- Chronic use of corticosteroids or other medications affecting bone density and healing;
- History of cancer treatment involving radiation to the lower extremities during growth years.
- Poor nutritional status during critical growth periods, particularly calcium and vitamin D deficiency.
Biomechanical factors:
- Pre-existing scoliosis or spinal asymmetry, which compounds the effects of leg length differences.
- Significant muscle imbalances or weakness on one side of the body.
- Joint hypermobility or ligamentous laxity reducing structural stability.
- Previous compensatory movement patterns from other injuries.
Pregnancy-related factors:
- Maternal infections during pregnancy affecting fetal bone development.
- Premature birth with associated complications.
- Birth trauma or difficult delivery affecting hip or leg positioning.
Psychosocial factors:
- Stress and anxiety can heighten pain perception and reduce adaptation capacity.
- Poor body awareness or kinesthetic sense, preventing early recognition of developing asymmetries.
- Limited access to healthcare for early intervention.
When you know the risk factors, it’s easier to get proactive screenings and early orthotic interventions before significant compensatory problems develop.
How Is Leg Length Discrepancy Diagnosed?

Diagnosing leg length discrepancy accurately requires a combination of clinical examination and imaging studies. These avenues determine both the presence and magnitude of the difference, as well as whether it's structural or functional.
Clinical Assessment
The diagnostic process typically starts with a thorough medical history, including questions about symptoms, family history, previous injuries, surgeries, and developmental concerns. During the physical examination, your healthcare provider observes your posture and gait, looking for limping, pelvic tilting, or compensatory movement patterns.
The block test is a simple yet effective clinical measurement: blocks of varying heights are placed under the shorter leg until the pelvis appears level, with the block height indicating the approximate discrepancy. Direct tape measurements from the anterior superior iliac spine (hip bone) to the medial malleolus (ankle bone) provide another clinical estimate. The provider also assesses spine curvature, shoulder height, hip and knee range of motion, and muscle strength on both sides.
Imaging Studies
While clinical measurements provide useful estimates, imaging confirms the diagnosis and determines whether the discrepancy is structural or functional. The scanogram X-ray is considered the gold standard for measuring structural leg length discrepancy. This specialized X-ray captures the hips, knees, and ankles in one image with a ruler superimposed directly on the film, allowing precise bone measurements with minimal error (typically within 1-2mm accuracy).
Orthoroentgenograms use three separate X-rays (one each of hips, knees, and ankles) with a ruler included in each image, allowing segment-by-segment bone measurement. EOS imaging, available in select facilities, uses low-dose radiation to create full-body standing images from front and side views, providing excellent visualization of overall alignment and bone length with reduced radiation exposure.
CT scanograms offer extremely precise measurements through cross-sectional imaging and are particularly useful when deformities make it difficult to interpret standard X-rays. For children still growing, an X-ray of the hand and wrist determines bone age (skeletal maturity), helping predict remaining growth and future discrepancy at skeletal maturity—essential information for surgical planning.
How Is Leg Length Discrepancy Treated?

There’s no one-size-fits-all treatment for leg length inequality. Approaches depend on the magnitude of the discrepancy, whether it's structural or functional, the patient's age and growth potential, symptom severity, and impact on daily function. Management ranges from simple observation to complex surgical interventions, with custom orthotics playing a central role in non-surgical treatment.
Observation and Monitoring
For children with small discrepancies (less than 1cm) who are still growing, or those with recent growth plate injuries, watchful waiting with regular monitoring may be appropriate. The discrepancy may self-correct as growth continues, remain stable without causing symptoms, or progress in predictable patterns that inform future treatment decisions. Regular follow-up appointments are important to track changes through serial measurements and imaging. If the discrepancy worsens or symptoms develop, intervention is initiated.
Physical Therapy and Manual Therapy
Conservative rehabilitation is often effective for functional leg length discrepancies resulting from muscular imbalances, pelvic misalignment, or joint restrictions. Physical therapy focuses on stretching tight muscles (particularly hip flexors, hamstrings, and piriformis), strengthening weak stabilizers around the hips and core, and improving overall flexibility and range of motion. Manual therapy techniques, including joint mobilization and soft tissue release, help restore proper alignment.
Chiropractors can be helpful in providing spinal adjustments and pelvic realignment to address functional discrepancies. For some patients with functional LLD, these conservative approaches can completely resolve the apparent leg length difference and eliminate the need for orthotic lifts.
Orthotic Management for Leg Length Discrepancy

Custom orthotic insoles for leg length discrepancy are the primary non-surgical treatment for structural LLD and provide supportive therapy for functional discrepancies. At PrimeCare, we specialize in creating precisely calibrated orthotic solutions tailored to each individual's specific needs.
Understanding Orthotic Lifts
How do insoles for leg length discrepancy work? They add height under the shorter leg to level the pelvis, realign the spine, and normalize gait patterns. The amount of lift required depends on the measured discrepancy and how well your body has already adapted to the difference. Keep in mind that the prescribed lift height doesn't always equal the measured anatomical difference—providing the full measured discrepancy immediately, especially in long-standing cases, can be poorly tolerated and create new problems.
Types of Leg Length Discrepancy Lifts
For discrepancies under 10mm, a full-length orthotic insole for the shorter leg with built-in heel elevation often suffices. These fit inside regular shoes with adequate depth and provide lift, along with arch support and cushioning.
Heel lifts or heel orthotics for leg length discrepancy, ranging from 4mm to 15mm, can be added inside shoes under the existing insole or combined with custom orthotics for a greater total lift. These are especially helpful for fine-tuning or temporary adjustments.
For moderate discrepancies (10-30mm), combined approaches are the most effective: a custom orthotic insert for leg length discrepancy providing 8-10mm of lift inside the shoe in addition to external shoe modifications adding height to the sole. This distributes the correction between inside and outside the shoe, helping to maintain the shoe’s comfort and fit.
Large discrepancies (over 30mm) typically require external shoe sole modifications, where a cobbler or orthotist adds layers to the shoe's outsole, sometimes including a rocker bottom for easier rolling through the gait cycle. For very large discrepancies, ankle-foot orthoses (AFOs) with built-in lifts or specialized prosthetic-type devices may be needed.
Full-Length vs. Heel Lifts
Research and clinical experience reveal that full-length insoles for shorter leg correction provide superior outcomes compared to heel-only lifts for moderate to large discrepancies. Full-length orthotic insoles for leg length discrepancy offer support throughout the entire foot, maintain proper arch position under the added weight of the lift, and distribute pressure more evenly. Heel lifts alone can create a forward pitch, increasing forefoot pressure and causing metatarsal pain, especially with heights exceeding 6-8mm.
Gradual Lift Adaptation

For congenital discrepancies where the body has compensated since childhood, we’ve found that introducing a lift gradually is essential. At PrimeCare, our team typically starts with 50-70% of the measured discrepancy and increases by 3-5mm increments every 4-6 weeks. This pace allows soft tissues to adapt to the changing alignment, minimizes discomfort, and reduces the risk of creating new problems in previously compensated areas.
For post-surgical discrepancies (such as after hip or knee replacement), the full correction can often be provided immediately since the discrepancy is new and no long-standing compensations exist.
Custom vs. Off-the-Shelf Solutions for Leg Length Discrepancy
While generic shoe inserts for leg length differences are available, custom orthotics for leg length discrepancy offer significant advantages. At PrimeCare, our pedorthists perform comprehensive gait analysis and foot biomechanics assessment, create custom foot molds ensuring proper arch support and pressure distribution, calibrate precise lift heights based on your specific needs, and design orthotics that fit your shoes and lifestyle. We use advanced materials providing both support and shock absorption, and can easily modify or adjust the orthotics as your needs change.
Shoe Considerations
How successful orthotic treatment is depends partly on the appropriate footwear. Shoes should have adequate depth to accommodate the orthotic without creating pressure on the top of the foot, removable insoles to make room for custom orthotics, and sturdy construction to maintain the orthotic in its proper position.
For significant lifts, you may need to adjust the shoe on the longer leg (trimming the insole or choosing a lower-profile shoe) to maintain equal overall height. Our team at PrimeCare provides specific footwear recommendations based on your orthotic prescription and activity requirements.
Footwear Modifications

Beyond internal orthotics, external shoe modifications address larger discrepancies. A cobbler or certified pedorthist can add sole lifts to the outside of the shoe, typically in 5-10mm increments, with rocker or wedge modifications to maintain natural gait patterns. For discrepancies exceeding 2cm, the lift may be split between the heel and sole to maintain a normal shoe profile.
Surgical Treatment Options
When non-surgical approaches prove insufficient or the discrepancy is severe (typically over 2-3cm), surgical correction may be considered. The approach depends on the patient's age, remaining growth, and the magnitude of correction needed.
Epiphysiodesis (Growth Modulation)
For children still growing, this procedure slows or stops growth in the longer leg by temporarily or permanently fusing the growth plate. A small implant or surgical ablation prevents further lengthening of the longer side, allowing the shorter leg to "catch up" over several years. Precise timing for this procedure is critical — it must be performed with enough growth remaining to achieve the desired correction, but not so early that the shorter leg eventually becomes longer.
Limb Lengthening

Various surgical techniques can lengthen the shorter leg through controlled bone distraction. The bone is surgically divided, and an external fixator (metal frame) or internal lengthening nail gradually separates the bone segments by approximately 1mm per day. New bone forms in the gap over several months. While effective, limb lengthening is complex and requires multiple surgeries, months of wearing the device, intensive physical therapy, and carries risks of infection, nerve damage, and joint stiffness.
Limb Shortening
For skeletally mature patients, the longer leg can be surgically shortened by removing a segment of bone, then using plates, screws, or rods to stabilize it while healing. This approach is faster than lengthening but permanently reduces overall height. It's typically reserved for discrepancies under 5cm and when the patient's height comfortably allows shortening.
Surgical decisions aren’t taken lightly, and they involve complex calculations considering current discrepancy, predicted discrepancy at skeletal maturity (for children), patient height and growth potential, activity level and goals, and psychological factors. A multidisciplinary team, including orthopedic surgeons, pedorthists, physical therapists, and sometimes psychologists, collaborates on surgical planning to ensure it’s the best option.

.svg)
.svg)



