Proximal femoral focal deficiency (PFFD) is a rare birth defect where the thigh bone is abnormally short or absent. At PrimeCare, we create individualized restoration plans to address hip and knee instability from birth, building high-performance prosthetics to equalize limb length and restore natural movement. Our facility specializes in the complex fabrication of sockets and joints for these unique skeletal structures.
Primary Characteristics of Proximal Femoral Focal Deficiency (PFFD)
Proximal femoral focal deficiency (PFFD) is a condition where a child is born with a shortened or incomplete thigh bone. The word "proximal" means the part of the bone closest to the hip, where the defect usually starts. Even though the foot and lower leg might look normal, they sit much higher up because the femur didn’t grow to its full length. As a result, this may make the hip and knee joints weak or unstable.
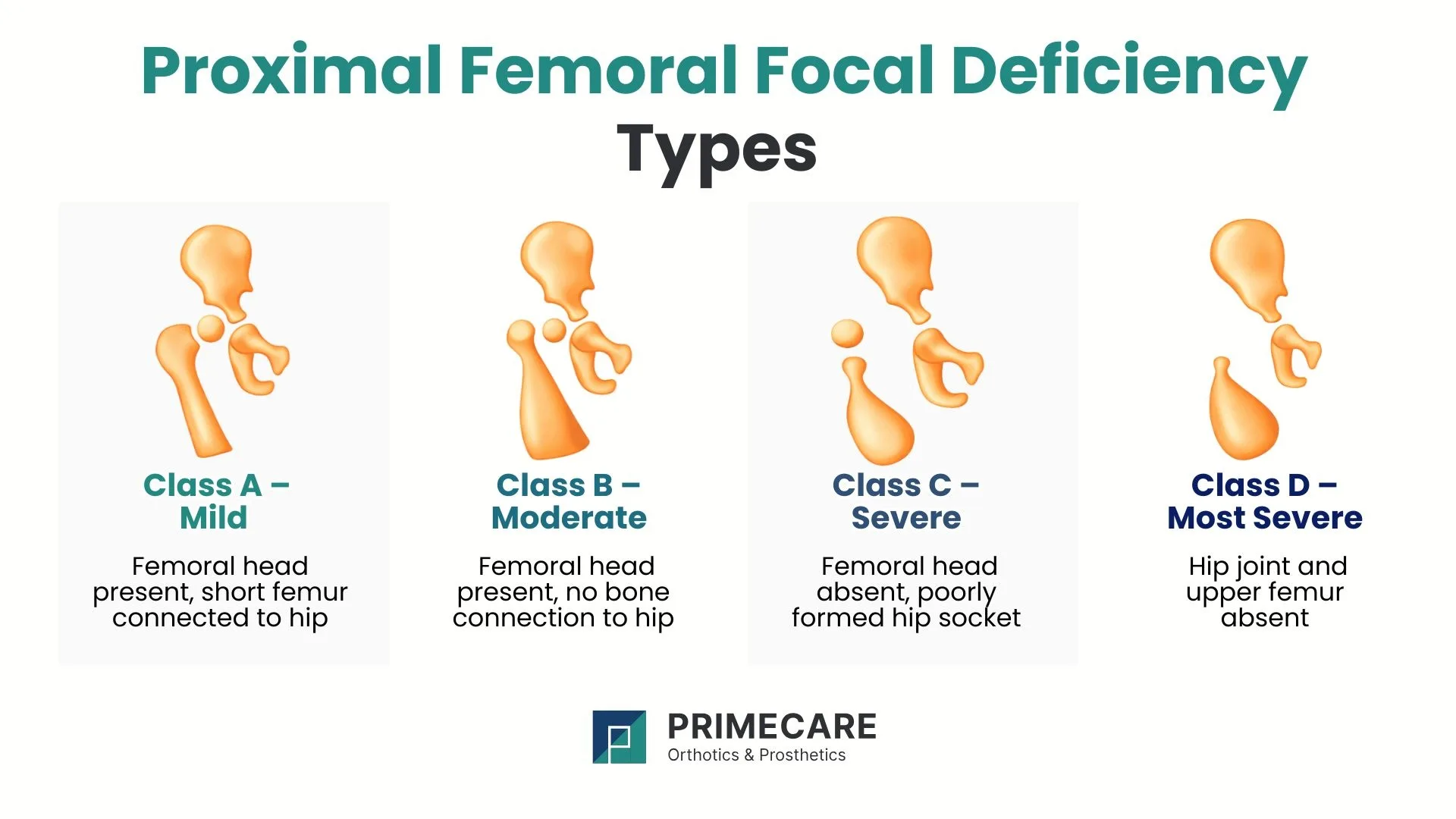
Established Classification Types of PFFD
Medical professionals generally use the Aitken Classification to categorize the severity of proximal femoral focal deficiency (PFFD). This system uses four distinct categories:
- Class A: The femoral head is present within the hip socket. A short femur exists, but a bony or cartilaginous connection remains between the hip and the shaft.
- Class B: The femoral head is present, and the hip socket (acetabulum) is well-formed, but there is no bony connection between the femur and the hip joint.
- Class C: The hip socket is severely underdeveloped, and the femoral head is either absent or fails to harden into bone. The femur itself is significantly shortened.
- Class D: The most severe form, characterized by the complete absence of the hip joint and the proximal femur. Only a small portion of the bone near the knee may remain.
These specific categories allow technicians to align prosthetic components with the patient’s unique skeletal structure.
Visible Symptoms of Proximal Femoral Focal Deficiency
The clinical presentation of proximal femoral focal deficiency (PFFD) is usually evident immediately. The affected limb typically displays the following:
- Significant leg length discrepancy: The knee on the affected side resides much higher than the healthy knee.
- External rotation: The thigh and foot often turn outward.
- Joint instability: The hip and knee joints lack the ligamentous strength for standard weight-bearing.
- Flexion deformity: The hip may stay in a bent position.
- Associated deficiencies: Many children also experience fibular hemimelia (an absent or short calf bone) or foot deformities.
Clinical assessment of these specific physical markers allows PrimeCare to design a restorative plan that factors in leg length and joint alignment to achieve long-term mobility.
Developmental Causes of Proximal Femoral Focal Deficiency
According to medical data, the deficiency develops between the fourth and eighth week of pregnancy, during early limb formation. While no single cause has been identified, contributing factors may include:
- Disruption of the blood supply to the developing limb
- Environmental influences during early fetal development
- Isolated developmental anomalies unrelated to genetics
Because the genetic risk for future siblings is extremely low, PFFD is considered a random developmental condition rather than a hereditary or family-wide trait.
Is PFFD Genetic or Inherited?

The exact cause of proximal femoral focal deficiency (PFFD) remains a subject of clinical study. According to research, the condition is not typically hereditary, meaning it occurs sporadically and does not usually pass from parent to child. The prevalence of this condition is roughly 1 in 100,000 live births, making the occurrence exceptionally rare.
Dangers of Untreated Proximal Femoral Focal Deficiency
Failure to manage proximal femoral focal deficiency (PFFD) properly results in long-term physical and functional complications. Without intervention, the massive imbalance in leg length leads to:
- Severe scoliosis: The spine compensates for the tilted pelvis, which leads to permanent curvature.
- Early-onset osteoarthritis: Excessive stress on the "good" leg and the back causes premature joint wear.
- Mobility restrictions: Inability to walk with a level gait prevents participation in standard physical activities.
- Psychosocial impact: Visible limb differences and limited independence can affect a child’s social development and self-esteem.
The main motivation behind early prosthetic intervention is preventing these secondary complications.

How Medical Teams Diagnose PFFD
Diagnosing proximal femoral focal deficiency (PFFD) often starts during prenatal ultrasound scans. After birth, doctors confirm the condition through:
- Physical examination: Assessment of the range of motion and the degree of shortening.
- X-ray imaging: Determination of the presence of the femoral head and the state of the hip socket.
- MRI scans: Evaluation of the soft tissues, ligaments, and un-ossified cartilage that may not appear on X-rays.
- Gait analysis: Observation of how the child moves once they reach standing age to plan for future devices.
Detailed diagnostic images serve as the blueprint for custom-fabricated mobility solutions.
Surgical Variants for Proximal Femoral Focal Deficiency
Surgery is often a foundational step in improving the limb’s function before or alongside prosthetic use. Common surgical options include:
- Hip and knee stabilization: Procedures to deepen the hip socket or tighten ligaments, which offers a stronger base for weight-bearing.
- Ilizarov limb lengthening: For mild cases, doctors use external fixators to slowly stretch the femur. This is a multi-stage process.
- Femoral-pelvic fusion: In cases with severe hip instability, surgeons may fuse the femur to the pelvis to create a stable, non-moving base for a prosthesis.
- Rotationplasty: A complex procedure where the ankle joint is turned backward to act as a functional knee joint, increasing control over an artificial limb.
Surgical outcomes often determine the specific type of prosthetic socket and joint selection.
Advanced Prosthetic Care for Proximal Femoral Focal Deficiency

To manage proximal femoral focal deficiency (PFFD), equalizing limb length is the priority. While surgery can stabilize joints, prosthetic intervention is the main solution for severe deficiencies.
Above-Knee (AK) Prosthetics
In cases where the femur is extremely short, the biological knee sits too high to function as a joint. PrimeCare builds above-knee prostheses that include a mechanical knee joint at the correct height to achieve a natural-looking gait and fluid movement.
Hip Disarticulation Prosthetics
In severe cases of PFFD where the femur is absent or unable to support weight-bearing, hip disarticulation prosthetics provide a comprehensive solution. These systems incorporate a hip joint mechanism along with knee and foot components, allowing upright ambulation and improved balance when limb preservation is not feasible.
Immediate Post-Operative Prosthetics (IPOP)
When surgical amputation or limb-modifying procedures are needed, an Immediate Post-Operative Prosthesis may be used in early recovery. IPOP systems support early standing, edema control, and a smoother transition to a definitive prosthetic limb.
Our prosthetic designs focus on maximum comfort and high-level durability to endure daily life.
Orthotic Braces for Proximal Femoral Focal Deficiency

Not every patient needs a full prosthesis right away. Specialized orthotic braces play a significant role in the management of proximal femoral focal deficiency.
- Knee-ankle-foot orthoses (KAFO): These braces offer external stability to a weak knee or ankle, which allows the patient to bear weight without limb buckle.
- Hip abduction braces: Often used after surgical procedures, these braces hold the hip in the correct position for proper healing and joint alignment.
- Custom night splints: These help maintain the range of motion and prevent muscle contraction in a bent position.
PrimeCare produces high-quality braces in New Mexico that bridge the gap between surgical recovery and full prosthetic use.
Perspective Outcome for PFFD Treatment
The outlook for individuals with proximal femoral focal deficiency is positive with early and consistent care. Modern prosthetic technology allows most patients to achieve full independence.
In fact, many individuals with PFFD lead active lives, participate in athletics, and hold demanding careers. The combination of early joint stabilization and advanced limb design ensures that the physical limitation doesn’t dictate the person's potential.
Treatment continues to evolve, and ongoing advancements in carbon fiber and robotics continue to improve the long-term quality of life for clients.

.svg)
.svg)



